- Home
- ServSafe
- Food Protection Manager
- ServSafe-Manager
- ServSafe Manager Exam Questions and Answers
ServSafe-Manager ServSafe Manager Exam Questions and Answers
What level of involvement do food workers have in executing a master cleaning schedule?
Options:
Rare
Planning
Voluntary
Mandatory
Answer:
DExplanation:
In a professional kitchen, sanitation is not the sole responsibility of the management; it is a shared duty that requires the active participation of every employee. The execution of a Master Cleaning Schedule isMandatoryfor all food workers. While the Person in Charge (PIC) or manager is responsible for the creation, planning, and oversight of the schedule, the actual labor of cleaning and sanitizing the facility must be integrated into the daily routines of the staff. ServSafe defines the master cleaning schedule as a roadmap that specifies what to clean, when to clean it, who is responsible, and how the task should be performed.
Mandatory involvement ensures that the facility does not rely on "voluntary" (Option C) or occasional "rare" (Option A) efforts, which often lead to neglect and the buildup of grease, dirt, and pests. Every worker must understand that cleaning as they go and completing assigned tasks on the schedule are non-negotiable job requirements. This involvement is critical because food workers are the ones interacting with the equipment and surfaces most frequently. If a worker fails to follow the schedule, biofilm can develop on food-contact surfaces, and non-food contact areas (like floors and drains) can become breeding grounds forListeriaor pests. Managers must provide the necessary tools, chemicals, and time for staff to fulfill these duties. Furthermore, the mandatory nature of the schedule allows for accountability; managers can verify that tasks were completed and sign off on the logs. This disciplined approach to facility maintenance is a key indicator of a strong food safety culture and is essential for passing health inspections and protecting public health.
A food establishment must have specific procedures for employees to follow when cleaning up which of the following substances?
Options:
Mold and mildew
Vomit and diarrhea
Food spills and beverage machine leaks
Rodent droppings and dead cockroaches
Answer:
BExplanation:
According to the FDA Food Code and the ServSafe Manager curriculum, every food establishment is required to have a formal, written plan for the cleanup ofvomit and diarrhea. This requirement ex1ists because these substan2ces are primary vehicles3for the transmission ofNorovirus, which is highly contagious and the leading cause of foodborne illness in the United States. Norovirus can be aerosolized (spread through the air) when a person vomits, and it can survive on surfaces for weeks if not properly disinfected.
The written procedures must detail how employees will minimize the spread of contamination to food, surfaces, and other people. This typically involves using a "Body Fluid Cleanup Kit" that includes personal protective equipment (PPE) such as disposable gloves, a gown, and a face mask. The cleanup process requires the use of a high-concentration disinfectant (such as a 1,000–5,000 ppm chlorine solution) rather than standard kitchen sanitizers, which are often too weak to kill Norovirus. The plan must also specify how to dispose of contaminated materials and how to handle the "exclusion" of the sick individual. While cleaning mold (Option A), spills (Option C), or pest evidence (Option D) is important for general sanitation, the legal mandate for aspecific written procedureis focused on Norovirus containment to prevent massive outbreaks. Managers are responsible for training all staff on these protocols before an incident occurs.
When the water supply has been disrupted due to a natural disaster, an acceptable alternative is
Options:
buying commercially bottled drinking water.
sanitizing water with a 50-50 mixture of bleach.
securing water from a private well tested every 2 years.
using clean water from the air conditioning system.
Answer:
AExplanation:
A disruption in the water supply is considered animminent health hazard. Because water is essential for handwashing, cooking, and sanitizing, an establishment cannot operate safely without a potable (drinkable) source. According to the ServSafe Manager curriculum, if the municipal supply fails, the only acceptable short-term alternative5for drinking and food preparation iscommercially bottled drinking waterfrom an approved source.
Other options are highly unsafe: a 50-50 bleach mixture (Option B) is toxic and would cause chemical poisoning. Private wells (Option C) must be tested at least annually, not every two years, and may not be sufficient during a disaster. Water from an air conditioning system (Option D) is non-potable and potentially contaminated with mold and chemicals. If an establishment uses bottled water, it must also address other needs, such as using single-service (disposable) plates and utensils to avoid the need for dishwashing and providing portable handwashing stations or hand sanitizer (though the latter is only a temporary measure). If safe water cannot be secured for all essential tasks, including restroom use and handwashing, the manager must close the operation until the water supply is restored and cleared by the regulatory authority.
A chemical sanitizing solution's effectiveness depends on the
Options:
water hardness, pH, and temperature of the solution.
color, odor, and scent of the solution.
type of test strips used to test the solution.
number of surfaces to be sanitized with the solution.
Answer:
AExplanation:
The chemical process of sanitizing is not as simple as just mixing chemicals with water. According to ServSafe, the effectiveness of a sanitizer (such as chlorine, iodine, or quaternary ammonium) is determined by several environmental factors, specificallywater hardness, pH, and temperature. Each of these factors can significantly impact the chemical's ability to kill pathogens. Water hardness refers to the amount of minerals (like calcium and magnesium) in the water; high mineral content can neutralize some sanitizers, particularly "Quats," making them ineffective. The pH of the water also dictates how stable and active a chemical remains; if the pH is too high or too low, the chemical reaction needed to kill bacteria may not occur.
Temperature is equally vital. Most chemical sanitizers have a "sweet spot" temperature (often between $75^{\circ}F$ and $120^{\circ}F$ depending on the chemical). If the water is too hot, the chemical may evaporate too quickly; if it is too cold, the chemical action slows down, failing to sanitize within the required contact time. While test strips (Option C) are used tomeasureconcentration, they do not dictate theeffectivenessitself. Color and odor (Option B) are unreliable indicators of strength. To ensure safety, managers must obtain a water quality report for their facility and check the manufacturer's label for the specific requirements of the sanitizer they are using. Using a test kit is the only way to verify that the concentration (measured in parts per million or ppm) is correct given the specific hardness, pH, and temperature of the local water supply. This verification is a core part of "Cleaning and Sanitizing" and is heavily scrutinized by health inspectors.
In general, pathogens grow very slowly or not at all at pH levels below
Options:
4.6.
5.0.
6.0.
6.4.
Answer:
AExplanation:
Bacteria require specific conditions to grow, often remembered by the acronymFAT TOM(Food, Acidity, Temperature, Time, Oxygen, Moisture). Acidity is measured on a pH scale from 0 to 14.0. Most foodborne pathogens grow best in food that is slightly acidic to neutral, typically between a pH of 4.6 and 7.5. ServSafe and the FDA Food Code identify4.6as the critical "cutoff" point for safety.
When the pH level of a food is below 4.6 (highly acidic), it creates an environment that is too hostile for most pathogenic bacteria, such asClostridium botulinum, to grow and produce toxins. This is why highly acidic foods like lemons, limes, and many vinegars are generally not considered TCS foods. In food preservation, such as pickling or fermenting, the goal is often to lower the pH of the food below this 4.6 threshold to make it shelf-stable. Conversely, foods with a pH above 4.6, such as meat, milk, and most vegetables, require strict time and temperature control because their low acidity allows for rapid bacterial multiplication. Managers must be aware of the pH of the items they serve, especially when dealing with specialized processes like "reduced oxygen packaging" (ROP) or acidified rice for sushi, where maintaining a safe pH is a critical control point.
A label on foods prepared and packaged onsite for retail sales must list which information?
Options:
A copy of the recipe used to prep the product
A list of all ingredients used in descending order by weight
Inspection score of the prep facility
Use-by dates that are 5 days after product prep
Answer:
BExplanation:
When a food establishment packages food for retail sale (such as a "grab-and-go" cooler), it must comply with strict labeling requirements mandated by the FDA Food Code. The label must include the common name of the food, the quantity (weight), the name and place of business of the manufacturer, and, crucially, alist of all ingredients in descending order by weight. This transparency is vital for consumer safety, particularly regarding food allergies.
The label must also clearly identify any of theBig 9 major allergenscontained in the food. If an ingredient (like bread) contains other sub-ingredients, those must also be listed. Option A is incorrect because the specific recipe is proprietary and not required for a safety label. Option C is incorrect as inspection scores are public record but not required on food labels. Option D is incorrect because the standard shelf life for TCS food is 7 days, not 5, and the specific date must be calculated based on the earliest expiring ingredient. Proper labeling allows guests to make informed decisions and protects the establishment from liability in the event of an allergic reaction. Managers must verify that every packaged item is accurately labeled before it is placed in the retail area to ensure compliance with both federal and local health laws.
Which action should a food handler take if a sanitizing solution has weakened after 2 hours?
Options:
Add hot water.
Add more sanitizer.
Increase the contact time.
Replace the entire solution.
Answer:
DExplanation:
Maintaining the correct concentration of a chemical sanitizing solution is a fundamental requirement of the "Cleaning and Sanitizing" domain. Over time, sanitizing solutions in buckets or three-compartment sinks lose their effectiveness due to several factors: the introduction of organic matter (food bits and grease), evaporation, and the "neutralizing" effect of leftover detergents or hard water minerals. According to ServSafe, once a solution has weakened—meaning its concentration has dropped below the manufacturer's recommended parts per million (ppm)—it must bereplaced entirely.
Adding more sanitizer (Option B) is incorrect because the existing solution is likely already "loaded" with organic soil, which binds to the active chemicals and renders them ineffective. Simply adding more chemical does not remove the soil that is inhibiting the sanitizer's performance. Increasing contact time (Option C) is also unsafe because there is no way for a food handler to accurately calculate how much extra time would compensate for a sub-standard concentration. To verify the strength of the solution, food handlers must use atest kit(test strips) designed for the specific sanitizer being used (e.g., Chlorine, Quat, or Iodine). The solution should be checked frequently and replaced whenever it becomes visibly dirty or fails the test strip check. This ensures that pathogens are actually being reduced to safe levels. Proper sanitation is a non-negotiable barrier against foodborne illness, and using fresh, clean, properly concentrated chemicals is the only way to guarantee safety.
When should food handlers use hand antiseptics?
Options:
Instead of washing hands
Before washing hands
After washing hands
After putting on gloves
Answer:
CExplanation:
Hand antiseptics (hand sanitizers) are often misunderstood in the foodservice industry. According to the ServSafe Manager curriculum and the FDA Food Code, hand antiseptics arenever a substitute for handwashing. They must only be usedafterthe full handwashing process has been completed and the hands have been dried.
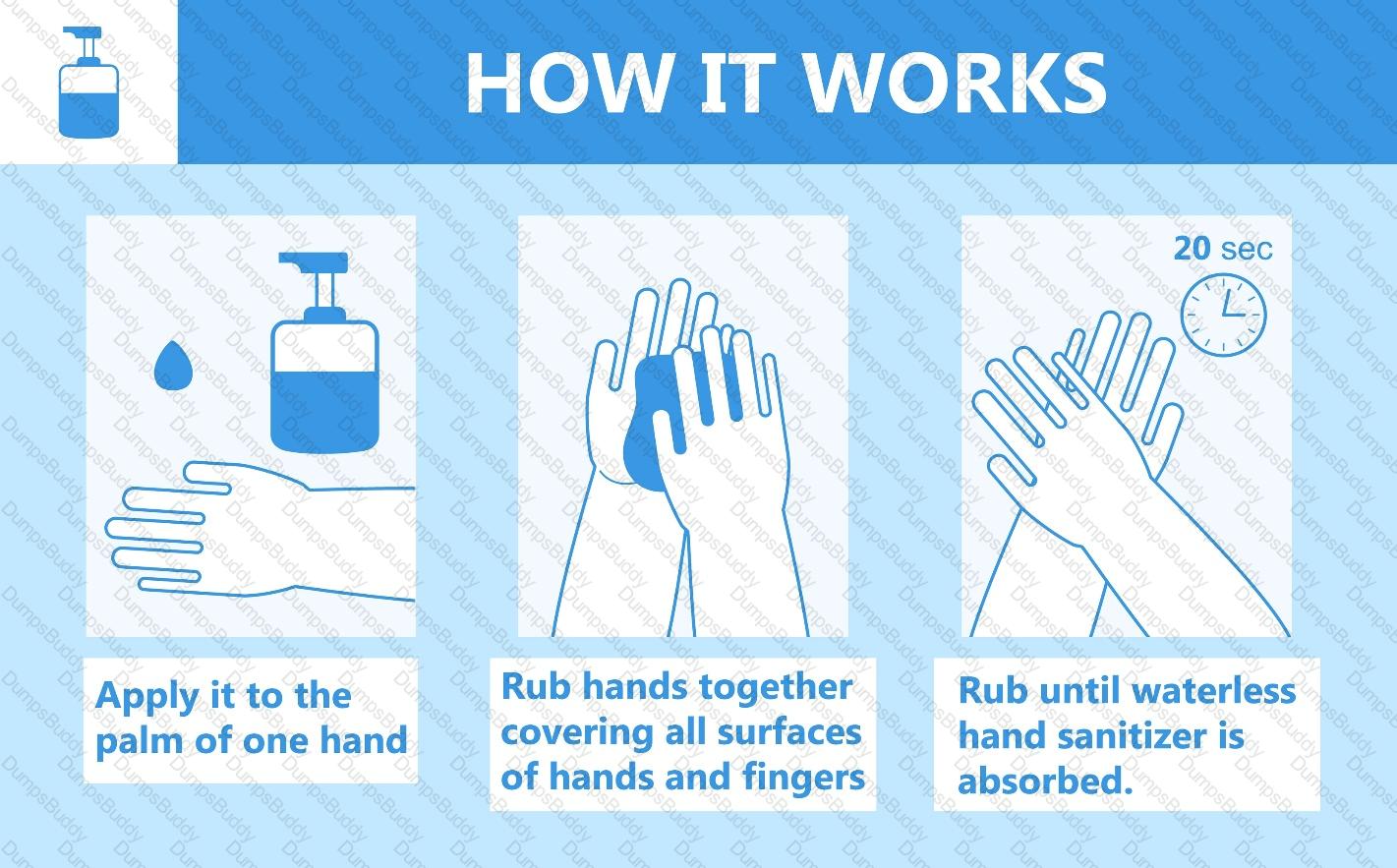 Image of handwashing vs. hand antiseptic use
Image of handwashing vs. hand antiseptic use
Shutterstock
The primary reason for this is that antiseptics are not effective at removing dirt, grease, or certain tough-to-kill pathogens likeNorovirusorHepatitis Aif the hands are soiled. Soap and water, combined with the mechanical friction of scrubbing, are required to physically lift and wash away these contaminants. An antiseptic used on dirty hands will simply be neutralized by the organic matter. Furthermore, the antiseptic used must be compliant with the FDA's "Code of Federal Regulations" for food contact. If an antiseptic is used, the food handler must allow it to completely air-dry before touching food or equipment to avoid chemical contamination. Using it before washing (Option B) is useless as the soap will wash it away, and using it instead of washing (Option A) is a major health code violation. Managers should view antiseptics as an "extra layer" of protection, but the core focus must always remain on rigorous, frequent handwashing at the appropriate times.
One method of denying pests access to an operation is to
Options:
install screens on windows and vents.
check deliveries after they are stored.
keep garbage cans clean and sanitized.
leave space between the floor and stationary equipment.
Answer:
AExplanation:
According to the ServSafe Manager curriculum, Integrated Pest Management (IPM) relies on three basic rules: deny pests access to the operation, deny pests food and shelter, and work with a licensed Pest Control Operator (PCO).Installing screens on windows and ventsis a primary physical barrier used to deny access. The FDA Food Code specifies that all openings to the outside must be protected against the entry of insects and rodents. Windows must be fitted with at least 16-mesh-to-the-inch screening, and vents must be properly covered.
Denying access also involves keeping exterior doors closed when not in use, installing air curtains (also called fly fans) above doorways, and sealing cracks in floors and walls with permanent sealant or copper mesh. Checking deliveriesafterthey are stored (Option B) is incorrect; deliveries should be inspectedbeforethey enter the facility to ensure pests are not being "hitched" in. While keeping garbage cans clean (Option C) is a vital sanitation practice, it serves to deny pestsfood and shelterrather than preventing their initial entry. Leaving space under equipment (Option D) is a requirement for "cleanability" so that staff can see signs of pests, but it does not stop them from entering the building. Managers must conduct regular facility "walk-throughs" to ensure that screens are not torn and that weather stripping on doors is intact. By maintaining a tight "envelope" around the building, the operation significantly reduces the biological hazards associated with pests like flies, which can carryShigellaand other pathogens.
Barracuda is a type of predatory tropical reef fish implicated as a source of which kind of toxin?
Options:
Fungal
Ciguatera
Histamine
Scombroid
Answer:
BExplanation:
Barracuda is the most common fish associated with Ciguatera Fish Poisoning. Ciguatera is a biological contaminant caused by a toxin produced by certain marine algae (dinoflagellates) found in tropical and subtropical waters. This toxin is fat-soluble and heat-stable, meaning it cannot be destroyed by cooking, freezing, or any other food preparation method. The toxin moves up the food chain through "bioaccumulation." Smaller herbivorous fish eat the algae, and then larger predatory reef fish—such as barracuda, grouper, snapper, and amberjack—eat those smaller fish, concentrating the toxin in their flesh.
When a human consumes a fish containing high levels of Ciguatoxin, they may experience severe symptoms, including nausea, vomiting, and neurological issues like a reversal of hot and cold sensations (where cold things feel hot and vice versa). Because the toxin cannot be detected by smell or sight and is not neutralized by heat, the only way to prevent Ciguatera poisoning is to purchase seafood only from approved, reputable suppliers. These suppliers monitor the waters where the fish are harvested and avoid areas known for Ciguatera outbreaks. Managers must be aware that predatory reef fish are a high-risk category and must strictly vet their seafood sources. This falls under the "Biological Contamination" section of "Providing Safe Food," highlighting that some hazards are inherent to the source of the food rather than a result of poor handling in the kitchen. Unlike Scombroid (Histamine) poisoning, which results from time-temperature abuse of fish like tuna or mahi-mahi, Ciguatera is a naturally occurring environmental hazard.
What must a food handler do with an uneaten basket of dinner rolls that was returned to the kitchen?
Options:
Throw the rolls away.
Donate the rolls to a local shelter.
Repurpose the rolls as croutons.
Allow employees to eat.
Answer:
AExplanation:
The FDA Food Code and ServSafe standards maintain a strict "No Re-service" policy to protect public health. Once food has been served to a customer, it is considered potentially contaminated and must never be served to another guest, repurposed for other dishes, or consumed by staff. Even if the dinner rolls appear untouched or were in a lined basket, they have been exposed to the customer’s environment. This includes potential exposure to airborne droplets from coughing or sneezing, and contact with unwashed hands or contaminated table surfaces.
The only exceptions to this rule are for "pre-packaged" foods that are still in their original, unopened, and pristine condition, such as individual cracker packets or sealed condiment pouches. Fresh bread, rolls, or open butter dishes do not meet this exception. Repurposing them as croutons (Option C) is a violation because the "cooking" process for croutons may not be sufficient to eliminate all pathogens introduced by the guest, and it establishes a dangerous precedent for food safety culture. Donating (Option B) or allowing staff to eat the rolls (Option D) also poses a risk of spreading foodborne illnesses likeNorovirusorStaphylococcus aureus. The only safe and compliant action is immediate disposal. Managers must train staff to recognize that the cost of a few rolls is negligible compared to the risk of a foodborne illness outbreak and the loss of customer trust.
==========
The water temperature in the first compartment of a three-compartment sink should be at least:
Options:
$110^{\circ}F$ ($43^{\circ}C$).
$135^{\circ}F$ ($57^{\circ}C$).
$171^{\circ}F$ ($77^{\circ}C$).
$180^{\circ}F$ ($82^{\circ}C$).
Answer:
AExplanation:
The three-compartment sink is the standard for manual warewashing in a professional kitchen. According to the FDA Food Code and ServSafe guidelines, the first sink is dedicated to washing. The water in this compartment must be at a minimum temperature of $110^{\circ}F$ ($43^{\circ}C$). This specific temperature is required because it is the threshold at which most commercial detergents become effective at breaking down food fats and greases. If the water is too cold, the detergent will not emulsify the grease, leaving a film on the dishes that prevents the sanitizer in the third sink from working effectively.
Managers must ensure that the sink is equipped with a thermometer to monitor the temperature throughout the cleaning process. If the water temperature drops below $110^{\circ}F$, it must be drained and refilled. The wash sink must also contain a detergent solution that is changed frequently to prevent the buildup of organic soil. For comparison, $171^{\circ}F$ (Option C) is the minimum temperature required for heat-based sanitizing in the third compartment if chemicals are not used, and $180^{\circ}F$ (Option D) is the required temperature for the final sanitizing rinse in a high-temperature commercial dishwasher. The $110^{\circ}F$ requirement for the first sink balances the need for chemical activation with the safety of the employee, as higher temperatures could cause burns during manual scrubbing. Maintaining this temperature is a critical "Active Managerial Control" point to ensure that the initial cleaning phase of warewashing is performed correctly, setting the stage for successful rinsing and sanitizing.
For a foodborne illness to be considered a confirmed outbreak, at least how many people must become sick?
Options:
1
2
4
6
Answer:
BExplanation:
According to the National Restaurant Association and the CDC standards used by ServSafe, a foodborne-illness outbreak is defined by three specific criteria. First,two or more peoplemust experience the same symptoms after eating the same food. Second, an investigation must be conducted by state or local regulatory authorities (such as the health department). Third, the outbreak must be confirmed by laboratory analysis, which identifies the specific pathogen (likeSalmonellaorNorovirus) in both the affected individuals and the food source.
Understanding this definition is vital for a Food Protection Manager because the reporting and investigation process only "confirms" an outbreak when that second person is linked to the event. A single case (Option A) is considered an "illness" but not an "outbreak," though it should still be taken seriously. There are rare exceptions—such as cases of Botulism or Scombroid poisoning—where even a single case may trigger an immediate emergency investigation, but for the general purposes of the ServSafe exam and standard regulatory definitions, the number is two. When a suspected outbreak occurs, the Manager’s role is to cooperate with the authorities, isolate any remaining suspected food (labeling it "Do Not Use/Do Not Discard"), and provide records like temperature logs and staff schedules. This helps investigators trace the source of the contamination, whether it was a failure in the "Flow of Food" (like improper cooling) or a sick employee. Proactive management and adherence to the FDA Food Code are designed to prevent these outbreaks from occurring by breaking the chain of contamination before it can affect multiple guests.
To transport cold time/temperature control for safety (TCS) foods, the maximum temperature of the food should be
Options:
$41^{\circ}F$ ($5^{\circ}C$).
$125^{\circ}F$ ($52^{\circ}C$).
$135^{\circ}F$ ($57^{\circ}C$).
$145^{\circ}F$ ($63^{\circ}C$).
Answer:
AExplanation:
In the "Flow of Food," the transportation phase is just as critical as the storage phase. When moving cold TCS foods—such as raw meats, poultry, dairy products, or cut melons—from a central kitchen to a satellite site or from a supplier to a restaurant, the internal temperature must remain at$41^{\circ}F$ ($5^{\circ}C$) or lower. This standard is mandated by the FDA Food Code to prevent pathogenic bacteria from entering the "Danger Zone" ($41^{\circ}F$ to $135^{\circ}F$), where they can multiply rapidly.
To maintain this temperature during transport, managers must use insulated, food-grade containers that can maintain cold temperatures for the duration of the trip. These containers must be cleaned and sanitized regularly. Additionally, the delivery vehicle itself should ideally be refrigerated. Upon arrival, the receiving party must immediately check the internal temperature of the food using a calibrated thermometer. If the food has risen above $41^{\circ}F$, it may need to be rejected, especially if the time spent at the elevated temperature cannot be verified. This requirement ensures that the "cold chain" remains unbroken. Options B, C, and D represent temperatures either within the Danger Zone or relevant to hot-holding/cooking, which are unsafe for cold transport. Managing transportation temperatures is a key component of a Food Safety Management System, particularly for catering operations or large school districts.
What is one approved way to preset utensils?
Options:
Wrap them in a napkin.
Preset indoors only.
Remove them at the end of the day.
Use only clear plastic utensils.
Answer:
AExplanation:
In the "Flow of Food," the service stage involves protecting utensils from contamination before they are used by the guest. According to the ServSafe Manager curriculum and the FDA Food Code, if a table is preset with silverware, the utensils must be protected from contamination.Wrapping them in a napkinis a primary approved method because it provides a physical barrier against dust, droplets from coughs or sneezes, and accidental contact by other guests or staff.
The regulation states that if utensils are preset and not wrapped, they must be removed and replaced when a new customer is seated, regardless of whether they appear to have been used. However, if the utensils are wrapped—such as in a "roll-up" where the napkin completely covers the items—they do not need to be swapped out if the previous guest did not use them. This is because the wrapping ensures the "sanitary status" of the items remains intact. Other approved methods include using a dispenser that only allows the user to touch the handle of the utensil. Options such as "presetting indoors only" (Option B) or "removing at the end of the day" (Option C) do not provide specific protection against contamination during the hours of operation. Proper handling of utensils is a critical part of the service phase to prevent the transmission of pathogens likeStaphylococcus aureusfrom human contact or environmental debris. Managers must ensure that staff who prepare these roll-ups wash their hands thoroughly before touching the clean silverware.
A food handler who is diagnosed with norovirus and is symptomatic should be
Options:
terminated as soon as possible.
excluded from the operation.
allowed to stay off work for 12 hours.
restricted from working around food.
Answer:
BExplanation:
The "Big 6" pathogens, which includeNorovirus, are highly contagious and can cause severe foodborne illness even in small doses. According to the ServSafe Manager curriculum, there is a strict distinction between "restricting" and "excluding" an employee. If an employee is diagnosed with Norovirus and is exhibiting symptoms (such as vomiting or diarrhea), the Person in Charge (PIC)must excludethem from the operation entirely. This means they are not allowed to be in the building, as they pose a high risk of spreading the virus through the air or surface contact.
Norovirus is the leading cause of foodborne illness in the U.S. and is often spread through the fecal-oral route. An excluded employee cannot return to work until they have been asymptomatic for at least24 hours(some jurisdictions require 48 hours) or provide a written release from a medical practitioner. Managers must report these diagnoses to the local regulatory authority. Simply "restricting" the employee (Option D)—which would mean letting them do non-food tasks like taking out the trash—is insufficient for Norovirus because of its high transmissibility. Correct management of sick employees is a primary component of "Active Managerial Control." By following the mandatory exclusion rules, the manager protects the health of the customers and the reputation of the business.
The Person in Charge (PIC) notices that a food handler has an infected wound on his or her hand. They must require the food handler to
Options:
get a release from a medical practitioner.
cover the wound with a waterproof bandage and single-use glove.
work in the office until the wound heals.
apply antibacterial cream to the wound.
Answer:
BExplanation:
According to the ServSafe Manager curriculum and the FDA Food Code, an infected wound, cut, or boil on a food handler's hand or wrist is a potential source ofStaphylococcus aureus. This pathogen is commonly found on the skin and can easily be transferred to food or food-contact surfaces. To mitigate this risk, the wound must be properly contained. The standard requirement is a "double barrier" system: the wound must first be covered with awaterproof, leak-proof bandage(such as a finger cot or rubber stall), and then asingle-use glovemust be worn over the bandage.
If the wound is on the arm, it must be covered with a waterproof bandage, but a glove is not required as the arm does not typically make direct contact with food. However, for wounds on the hand or wrist, the glove is mandatory. This is a "restriction" protocol. The employee can still work with food as long as the wound is completely covered and the barrier is maintained. If the wound cannot be properly covered (for example, if it is persistently oozing or if the employee cannot wear gloves), the PIC mustrestrictthe employee from working with exposed food, clean equipment, or utensils. This procedure ensures that biological contaminants from the infection do not enter the "Flow of Food." Managers must monitor these barriers throughout the shift to ensure the bandage stays dry and the glove remains intact.
An operation must hire a pest control operator who is
Options:
bonded.
licensed.
experienced.
insured.
Answer:
BExplanation:
Integrated Pest Management (IPM) is a critical part of maintaining a safe food facility. Pests such as cockroaches, rodents, and flies are not just a nuisance; they are biological hazards that carry pathogens likeSalmonella,Shigella, andE. coli. ServSafe Manager guidelines mandate that an operation must work with alicensed Pest Control Operator (PCO). While being bonded, insured, or experienced are positive business attributes, the legal and safety requirement focuses on the license.
A licensed PCO has the specialized training to handle restricted-use pesticides that are not available to the general public. They understand the behavior of pests and can develop a customized prevention and treatment plan that is safe for a food-handling environment. The FDA Food Code prohibits food handlers from applying their own pesticides because improper application can lead to chemical contamination of food and surfaces. A PCO will provide documentation of their visits, the chemicals used, and recommendations for facility repairs (such as sealing cracks or fixing floor drains). Managers are responsible for providing the PCO with access to the building and following through on their suggestions for "pest-proofing." This partnership is a proactive "Food Safety Management System" designed to deny pests food, water, and shelter before an infestation can take root.
Which is a way to prevent contamination of hot food on display in a self-service area?
Options:
Providing a handwashing sink for customers
Providing fresh plates for return visits by customers12
Assigning food handlers to follow customers through the self-service area34
Posting strongly worded signs about inappropriate customer behavior56
Answer:
BExplanation:
In a self-service or buffet environment, one of the greatest risks of cross-c9ontamination is "norovirus" and other path10ogens being transferred from used plates back to the communal serving utensils or the food itself. The FDA Food Code and ServSafe standards strictly require thatfresh plates must be provided for return visitsby customers. When a customer takes a "dirty" plate back to the buffet line, there is a high probability that the serving spoon or tong will touch the plate, which may have been contaminated by the customer's saliva or hands during their first course.
Establishments must post signs or use staff to remind customers to use a clean plate for every trip to the buffet. Additionally, the food must be protected by sneeze guards, which should be located 14 inches ($36$ centimeters) above the food and extend 7 inches ($18$ centimeters) beyond the food. While assigning handlers to monitor the line (Option C) is a good general practice for safety, the "fresh plate" rule is a specific, mandatory regulatory requirement. Providing handwashing sinks for customers (Option A) is helpful but does not prevent the specific plate-to-utensil contamination. Signs (Option D) are only effective if the rule—specifically the use of clean plates—is actively enforced. Managers are responsible for ensuring a sufficient supply of clean plates is always available at the start of the buffet line to encourage this safe behavior.
When cooling food, an acceptable alternative to the two-stage cooling method is to use a
Options:
blast chiller.
commercial cooler.
heavy-duty freezer.
fan blowing on food.
Answer:
AExplanation:
Cooling food safely is one of the most difficult tasks in a kitchen because it requires moving food through the "Danger Zone" ($135^{\circ}F$ to $41^{\circ}F$) quickly to prevent the growth of bacteria likeClostridium perfringens. The standard two-stage cooling method requires food to be cooled from $135^{\circ}F$ to $70^{\circ}F$ within two hours, and then from $70^{\circ}F$ to $41^{\circ}F$ in the next four hours. Anacceptable alternativeand a highly effective professional tool for this process is ablast chiller.
A blast chiller works by blowing high-velocity cold air over the food, removing heat much faster than a standard refrigerator can. This is the preferred method for large volumes of dense food like stews or thick sauces. Using a standard commercial cooler (Option B) for cooling large batches of hot food is dangerous because it cannot remove heat fast enough; the hot food will also raise the ambient temperature of the cooler, putting other stored foods at risk. A heavy-duty freezer (Option C) is not designed for cooling and can lead to uneven temperatures and "freezer burn" if not monitored. A fan (Option D) can be used as asupplementto an ice-water bath, but on its own, it is not an acceptable cooling method as it can blow contaminants onto the food. Other approved methods include using an ice-water bath, stirring food with an ice paddle, or adding ice as an ingredient. Managers must ensure that temperatures are logged during the cooling process to verify that safety thresholds are met.
Which of the following is evidence of deliberate tampering of food?
Options:
Labels are missing from food containers.
Sulfites are added to prevent browning of lettuce.
Protective seal or wrapper is missing from a food container.
Food employees are handling ready-to-eat foods with bare hands.
Answer:
CExplanation:
Food defense is the protection of food products from intentional contamination by biological, chemical, physical, or radiological agents. While "accidental" contamination (like a hair in a soup) is common, "deliberate tampering" is an act of sabotage. According to the ServSafe Manager guidelines and the FDA’sA.L.E.R.T.program, one of the most visible signs of tampering is amissing or broken protective seal or wrapperon a food container. These seals are designed to guarantee the integrity of the product from the manufacturer to the end-user. If a seal is broken, it suggests that an unauthorized individual may have had access to the contents.
Managers must train receiving staff to inspect all incoming deliveries specifically for signs of tampering. This includes checking for punctured packaging, leaking containers, or boxes that appear to have been resealed with non-factory tape. While missing labels (Option A) are a regulatory violation and bare-hand contact (Option D) is a hygiene failure, they do not necessarily indicate a malicious attempt to harm the public. Adding sulfites (Option B) is actually a prohibited practice for fresh produce in many jurisdictions, but it is a chemical additive issue rather than tampering. To mitigate the risk of deliberate contamination, the A.L.E.R.T. system suggests that managers:Assure products are from safe sources,Look and monitor the security of the facility,Employees (know who is in the building),Report and keep records, andThreat (know what to do if a threat occurs). Isolating and reporting any products with suspicious packaging is a mandatory step in protecting the business and its customers from intentional harm.
When receiving fresh meat, its temperature at the time of receipt must not be higher than
Options:
$32^{\circ}F$ ($0^{\circ}C$).
$41^{\circ}F$ ($5^{\circ}C$).
$55^{\circ}F$ ($13^{\circ}C$).
$70^{\circ}F$ ($21^{\circ}C$).
Answer:
BExplanation:
In the "Flow of Food," receiving is the first line of defense against foodborne illness. According to the ServSafe Manager curriculum and the FDA Food Code, all cold Time/Temperature Control for Safety (TCS) foods—including fresh meat, poultry, and seafood—must be received at an internal temperature of$41^{\circ}F$ ($5^{\circ}C$) or lower. This temperature is the upper limit of the safe cold-holding zone. Receiving meat above this temperature indicates that it has been subjected to time-temperature abuse during transport, which allows for the rapid multiplication of pathogens such asSalmonellaandE. coli.
When a delivery arrives, the Person in Charge (PIC) or a designated receiver must use a calibrated bimetallic stemmed thermometer or a thermocouple to check the internal temperature of the product. For meat and poultry, the probe should be inserted into the thickest part of the product. If the temperature exceeds $41^{\circ}F$, the shipment should be rejected and the incident documented in a receiving log. This practice is a critical component of Active Managerial Control, ensuring that only safe, high-quality ingredients enter the kitchen. While some items like shell eggs or milk have slightly higher receiving temperature allowances ($45^{\circ}F$), fresh meat must strictly adhere to the $41^{\circ}F$ standard. Maintaining the "cold chain" from the supplier to the refrigerator is essential for preventing the growth of microorganisms and extending the shelf life of the product.
If it is used frequently, a milkshake mixer must be cleaned and sanitized at least every how many hours?
Options:
2
4
6
8
Answer:
BExplanation:
According to the ServSafe Manager guidelines and the FDA Food Code, any food-contact surface that is in constant, frequent use must be cleaned and sanitized at a minimum interval of every four hours. This "four-hour rule" is based on the biological reality of bacterial growth. Under ideal conditions—moist environments with plenty of nutrients, like the milk and sugar residue found in a milkshake mixer—pathogenic bacteria can multiply to dangerous levels within this timeframe. By mandating a complete cleaning and sanitizing cycle every four hours, the operation effectively breaks the bacterial growth cycle before it reaches a "log phase" where the population explodes.
For a milkshake mixer, the process involves more than just a surface wipe. The equipment must be disassembled if necessary, washed with detergent in hot water, rinsed to remove soap film, and then treated with a chemical sanitizer (such as chlorine or quaternary ammonium) for the required contact time. If the environment is particularly warm—exceeding $70^{\circ}F$ ($21^{\circ}C$)—the risk of bacterial growth increases, but the four-hour standard remains the regulatory baseline for room-temperature operations. Managers are responsible for implementing this into the daily workflow, often using "timed" cleaning logs to verify compliance. Failure to sanitize frequently used equipment is a common critical violation during health inspections because it creates a direct path for cross-contamination. If the mixer is only used occasionally, it must still be cleaned and sanitized after each use or before switching to a different flavor that might contain allergens. This rigid schedule is a core component of Active Managerial Control, ensuring that the physical environment remains safe despite the high volume of food production.
A shipment of unbroken shell eggs should be rejected when the
Options:
eggs are not Grade A.
yolk does not break easily.
egg shells are soiled.
white of the egg clings to the yolk.
Answer:
CExplanation:
Receiving criteria for shell eggs are strict because eggs are a TCS food and can be a source ofSalmonella. According to ServSafe receiving standards, shell eggs must be clean and unbroken upon delivery. If theegg shells are soiled—meaning they have traces of manure, dirt, or feathers—the shipment must be rejected. Soiled shells indicate poor sanitary conditions at the farm or during packing, and the dirt on the outside of the shell can easily contaminate the egg when it is cracked or contaminate the hands of the food handler.
The quality of the egg (Option A), such as Grade AA, A, or B, is a matter of preference and recipe requirement rather than safety. A yolk that does not break (Option B) or a white that clings to the yolk (Option D) are actually signs of high-quality, fresh eggs; as eggs age, the whites become thinner and the yolks break more easily. From a safety perspective, the manager must verify that the eggs are received at an ambient air temperature of $45^{\circ}F$ ($7^{\circ}C$) or lower and that the shells are free of cracks and visible filth. Any eggs that are leaking or dirty pose a significant risk of cross-contamination in the refrigerator. Documenting the rejection and the reason (e.g., "soiled shells") is a key part of an operation's Food Safety Management System and ensures that only safe products enter the Flow of Food.


