- Home
- CBIC
- Infection Control
- CIC
- CBIC Certified Infection Control Exam Questions and Answers
CIC CBIC Certified Infection Control Exam Questions and Answers
It is determined that the Infection Prevention and Control Program has inadequate resources to accomplish the required tasks. What is the FIRST step?
Options:
Review studies and recommendations on resource allowances for staffing decisions
Contact hospitals in the region to determine their staffing guidelines
Schedule a meeting with supervisor to discuss current job duties
Update the Infection Prevention and Control Plan
Answer:
CExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that when an Infection Prevention and Control (IPC) Program identifies inadequate resources, the first and most critical step is internal assessment and communication. Scheduling a meeting with the supervisor to discuss current job duties allows the infection preventionist to clearly define workload demands, regulatory requirements, and gaps between assigned responsibilities and available resources.
This initial discussion establishes a shared understanding of scope of practice, priority tasks, and compliance obligations, such as surveillance, reporting, education, emergency preparedness, and performance improvement. The Study Guide highlights that resource justification must begin with a clear inventory of required functions versus available staffing, time, and tools. Without this foundational step, subsequent actions—such as benchmarking, literature review, or plan updates—lack context and organizational alignment.
Option A is an important later step, used to support justification once internal expectations and gaps are defined. Option B may provide benchmarking data but should not precede internal role clarification. Option D is premature, as program plans should be updated only after leadership agreement on scope, priorities, and resources.
For CIC® exam preparation, it is essential to recognize that effective advocacy for IPC resources begins with direct supervisor engagement, role clarification, and documentation of unmet needs. This structured approach aligns with leadership principles and ensures that requests for additional resources are credible, data-driven, and organizationally relevant.
Immediate use steam sterilization is NOT recommended for implantable items requiring immediate use because
Options:
the high temperature may damage the items.
chemical indicators may not be accurate at high temperatures.
results of biologic indicators are unavailable prior to use of the item.
the length of time is inadequate for the steam to penetrate the pack.
Answer:
CExplanation:
The correct answer is C, "results of biologic indicators are unavailable prior to use of the item," as this is the primary reason immediate use steam sterilization (IUSS) is not recommended for implantable items requiring immediate use. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, IUSS is a process used for sterilizing items needed urgently when no other sterile options are available, typically involving a shortened cycle (e.g., flash sterilization). However, for implantable items—such as orthopedic hardware or prosthetic devices—ensuring absolute sterility is critical due to the risk of deep infection. Biologic indicators (BIs), which contain highly resistant spores to verify sterilization efficacy, require incubation (typically 24-48 hours) to confirm the kill, but IUSS does not allow time for BI results to be available before the item is used (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.3 - Ensure safe reprocessing of medical equipment). This lack of immediate verification poses a significant infection risk, making IUSS inappropriate for implants, as per AAMI ST79 standards.
Option A (the high temperature may damage the items) is a consideration for some heat-sensitive materials, but modern IUSS cycles are designed to minimize damage, and this is not the primary reason for the restriction on implants. Option B (chemical indicators may not be accurate at high temperatures) is incorrect, as chemical indicators (e.g., color-changing strips) are reliable at high temperatures and serve as an immediate check, though they are not a substitute for BIs. Option D (the length of time is inadequate for the steam to penetrate the pack) is not the main issue, as IUSS cycles are optimized for penetration, though the shortened time may be a secondary concern; the unavailability of BI results remains the decisive factor.
The focus on biologic indicator results aligns with CBIC’s emphasis on ensuring the safety and sterility of reprocessed medical devices, particularly for high-risk implantable items (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). This recommendation is supported by AAMI and CDC guidelines, which prioritize BI confirmation for implants to prevent healthcare-associated infections (AAMI ST79:2017, CDC Sterilization Guidelines, 2019).
Over the past 6 months, a facility has noticed an increase in healthcare-associated pneumonias in ventilator-dependent patients in the NICU. There were eight healthcare-associated pneumonias among ventilated patients. Total ventilator days were 240. What was the ventilator-associated pneumonia rate for the NICU during the 6-month period?
Options:
33/1,000 ventilator days
30/1,000 ventilator days
3.3/1,000 ventilator days
3/1,000 ventilator days
Answer:
AExplanation:
The Certification Study Guide (6th edition) explains that device-associated infection rates are calculated using a standardized formula that expresses the number of infections per 1,000 device days. This allows comparison over time and between units with different patient volumes or device utilization.
The formula for ventilator-associated pneumonia (VAP) rate is:
(Number of VAPs ÷ Number of ventilator days) × 1,000
In this scenario, there were 8 ventilator-associated pneumonias and 240 ventilator days over the 6-month period.
8 ÷ 240 = 0.033
0.033 × 1,000 = 33.3 VAPs per 1,000 ventilator days
Rates are typically rounded to a whole number for reporting and benchmarking purposes, resulting in 33 per 1,000 ventilator days.
The study guide emphasizes that ventilator days—not patient days or admissions—are the correct denominator because they reflect time at risk for ventilator-associated infection. This approach ensures valid surveillance and supports accurate trend analysis and benchmarking.
The other answer choices represent incorrect calculations or decimal misplacement. Understanding rate calculations is a core CIC exam competency, particularly for interpreting device-associated infection data and guiding quality improvement initiatives in high-risk units such as NICUs.
==========
A city has a population of 150.000. Thirty new cases of tuberculosis (TB) were diagnosed in the city last year. These now cases brought the total number of active TB cases in the city last year to 115. Which of the following equations represents the incidence rate tor TB per 100.000 in that year?
Options:
(30 ÷ 150.000) x 100.000 = X
(30÷ 150.000) x 100 = X
(115 ÷ 150.000) x 100.000 - X
(115 ÷ 100.000) x 100 = X
Answer:
AExplanation:
The incidence rate is calculated using the formula:
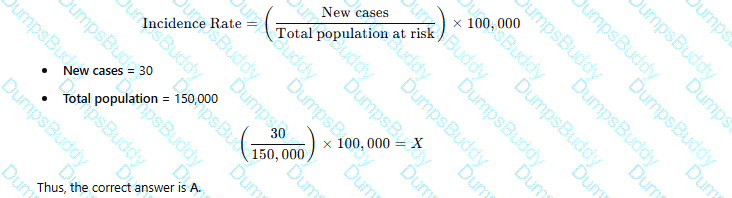
Why the Other Options Are Incorrect?
B. (30 ÷ 150,000) × 100 = X – Incorrect multiplier (should be 100,000 for standard incidence rate).
C. (115 ÷ 150,000) × 100,000 = X – 115 represents total cases (prevalence), not incidence.
D. (115 ÷ 100,000) × 100 = X – Uses the wrong denominator and multiplier.
CBIC Infection Control Reference
APIC defines the incidence rate as the number of new cases per population unit, typically per 100,000 people.
Two patients in a medical intensive care unit (ICU) and one patient in a surgical ICU have Aspergillus fumigatus cultured from sputum. An exterior construction project was started two weeks ago with demolition of an old office building one week ago. All of the following questions are important for the infection preventionist to ask EXCEPT:
Options:
“Have ventilation filters been changed according to the preventive maintenance schedule during construction?”
“Where are the air-intake units relative to these two ICUs?”
“Are there any healthcare personnel that have cared for both of these patients during their hospitalization?”
“Has Aspergillus fumigatus been cultured from these patients prior to construction?”
Answer:
CExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that Aspergillus infections associated with healthcare settings are most commonly environmentally acquired, particularly during construction, renovation, or demolition activities. Aspergillus fumigatus is an airborne mold, and transmission occurs through inhalation of spores, not via person-to-person contact.
In this scenario, the infection preventionist should focus on air handling systems and environmental controls, which makes options A, B, and D critical questions. Ensuring that ventilation filters are appropriately maintained (Option A) and evaluating the proximity of air-intake units to construction activities (Option B) are essential elements of an Infection Control Risk Assessment (ICRA). Asking whether Aspergillus was present before construction (Option D) helps determine whether this represents a construction-associated cluster rather than baseline colonization.
Option C is the least relevant because healthcare personnel do not transmit Aspergillus between patients. Unlike organisms spread via contact or droplets, Aspergillus spores are ubiquitous in dust and air and are introduced through environmental disruption. Therefore, evaluating shared staff assignments does not contribute meaningfully to identifying the source of exposure.
For CIC® exam preparation, it is critical to remember that construction-associated aspergillosis investigations focus on air quality, ventilation, and environmental controls—not staff transmission pathways.
A new hospital disinfectant with a 3-minute contact time has been purchased by Environmental Services. The disinfectant will be rolled out across the patient care 3-minute contact time has been purchased by Environmental Services. The disinfectant will be rolled out across the patient care areas. They are concerned about the high cost of the disinfectant. What advice can the infection preventionist provide?
Options:
Use the new disinfectant for patient washrooms only.
Use detergents on the floors in patient rooms.
Use detergents on smooth horizontal surfaces.
Use new disinfectant for all surfaces in the patient room.
Answer:
CExplanation:
The scenario involves the introduction of a new hospital disinfectant with a 3-minute contact time, intended for use across patient care areas, but with concerns raised by Environmental Services about its high cost. The infection preventionist’s advice must balance infection control efficacy with cost management, adhering to principles outlined by the Certification Board of Infection Control and Epidemiology (CBIC) and evidence-based practices. The goal is to optimize the disinfectant’s use while ensuring a safe environment. Let’s evaluate each option:
A. Use the new disinfectant for patient washrooms only: Limiting the disinfectant to patient washrooms focuses its use on high-touch, high-risk areas where pathogens (e.g., Clostridioides difficile, norovirus) may be prevalent. However, this approach restricts the disinfectant’s application to a specific area, potentially leaving other patient care surfaces (e.g., bed rails, tables) vulnerable to contamination. While cost-saving, it does not address the broad infection control needs across all patient care areas, making it an incomplete strategy.
B. Use detergents on the floors in patient rooms: Detergents are cleaning agents that remove dirt and organic material but lack the antimicrobial properties of disinfectants. Floors in patient rooms can harbor pathogens, but they are generally considered lower-risk surfaces compared to high-touch areas (e.g., bed rails, doorknobs). Using detergents instead of the new disinfectant on floors could reduce costs but compromises infection control, as floors may still contribute to environmental transmission (e.g., via shoes or equipment). This option is not optimal given the availability of an effective disinfectant.
C. Use detergents on smooth horizontal surfaces: Smooth horizontal surfaces (e.g., tables, counters, overbed tables) are common sites for pathogen accumulation and transmission in patient rooms. Using detergents to clean these surfaces removes organic material, which is a critical first step before disinfection. If the 3-minute contact time disinfectant is reserved for high-touch or high-risk surfaces (e.g., bed rails, call buttons) where disinfection is most critical, this approach maximizes the disinfectant’s efficacy while reducing its overall use and cost. This strategy aligns with CBIC guidelines, which emphasize a two-step process (cleaning followed by disinfection) and targeted use of resources, making it a practical and cost-effective recommendation.
D. Use new disinfectant for all surfaces in the patient room: Using the disinfectant on all surfaces ensures comprehensive pathogen reduction but increases consumption and cost, which is a concern for Environmental Services. While the 3-minute contact time suggests efficiency, overusing the disinfectant on low-risk surfaces (e.g., floors, walls) may not provide proportional infection control benefits and could strain the budget. This approach does not address the cost concern and is less strategic than targeting high-risk areas.
The best advice is C, using detergents on smooth horizontal surfaces to handle routine cleaning, while reserving the new disinfectant for high-touch or high-risk areas where its antimicrobial action is most needed. This optimizes infection prevention, aligns with CBIC’s emphasis on evidence-based environmental cleaning, and addresses the cost concern by reducing unnecessary disinfectant use. The infection preventionist should also recommend a risk assessment to identify priority surfaces for disinfectant application.
CBIC Infection Prevention and Control (IPC) Core Competency Model (updated 2023), Domain IV: Environment of Care, which advocates for targeted cleaning and disinfection based on risk.
CBIC Examination Content Outline, Domain III: Prevention and Control of Infectious Diseases, which includes cost-effective use of disinfectants.
CDC Guidelines for Environmental Infection Control in Healthcare Facilities (2022), which recommend cleaning with detergents followed by targeted disinfection.
Following recent renovations on an oncology unit, three patients were identified with Aspergillus infections. The infections were thought to be facility-acquired. Appropriate environmental microbiological monitoring would be to culture the:
Options:
Air
Ice
Carpet
Aerators
Answer:
AExplanation:
The scenario describes an outbreak of Aspergillus infections among three patients on an oncology unit following recent renovations, with the infections suspected to be facility-acquired. Aspergillus is a mold commonly associated with environmental sources, particularly airborne spores, and its presence in immunocompromised patients (e.g., oncology patients) poses a significant risk. The infection preventionist must identify the appropriate environmental microbiological monitoring strategy, guided by the Certification Board of Infection Control and Epidemiology (CBIC) and CDC recommendations. Let’s evaluate each option:
A. Air: Aspergillus species are ubiquitous molds that thrive in soil, decaying vegetation, and construction dust, and they are primarily transmitted via airborne spores. Renovations can disturb these spores, leading to aerosolization and inhalation by vulnerable patients. Culturing the air using methods such as settle plates, air samplers, or high-efficiency particulate air (HEPA) filtration monitoring is a standard practice to detect Aspergillus during construction or post-renovation in healthcare settings, especially oncology units where patients are at high risk for invasive aspergillosis. This aligns with CBIC’s emphasis on environmental monitoring for airborne pathogens, making it the most appropriate choice.
B. Ice: Ice can be a source of contamination with bacteria (e.g., Pseudomonas, Legionella) or other pathogens if improperly handled or stored, but it is not a typical reservoir for Aspergillus, which is a mold requiring organic material and moisture for growth. While ice safety is important in infection control, culturing ice is irrelevant to an Aspergillus outbreak linked to renovations and is not a priority in this context.
C. Carpet: Carpets can harbor dust, mold, and other microorganisms, especially in high-traffic or poorly maintained areas. Aspergillus spores could theoretically settle in carpet during renovations, but carpets are not a primary source of airborne transmission unless disturbed (e.g., vacuuming). Culturing carpet might be a secondary step if air sampling indicates widespread contamination, but it is less direct and less commonly recommended as the initial monitoring site compared to air sampling.
D. Aerators: Aerators (e.g., faucet aerators) can harbor waterborne pathogens like Pseudomonas or Legionella due to biofilm formation, but Aspergillus is not typically associated with water systems unless there is significant organic contamination or aerosolization from water sources (e.g., cooling towers). Culturing aerators is relevant for waterborne outbreaks, not for an Aspergillus outbreak linked to renovations, making this option inappropriate.
The best answer is A, culturing the air, as Aspergillus is an airborne pathogen, and renovations are a known risk factor for spore dispersal in healthcare settings. This monitoring strategy allows the infection preventionist to confirm the source, assess the extent of contamination, and implement control measures (e.g., enhanced filtration, construction barriers) to protect patients. This is consistent with CBIC and CDC guidelines for managing fungal outbreaks in high-risk units.
CBIC Infection Prevention and Control (IPC) Core Competency Model (updated 2023), Domain IV: Environment of Care, which recommends air sampling for Aspergillus during construction-related outbreaks.
CBIC Examination Content Outline, Domain III: Prevention and Control of Infectious Diseases, which includes environmental monitoring for facility-acquired infections.
CDC Guidelines for Environmental Infection Control in Healthcare Facilities (2022), which advocate air culturing to detect Aspergillus post-renovation in immunocompromised patient areas.
The infection preventionist (IP) collaborates with the Intravenous Therapy team to select the best antiseptic for use during the insertion of an intravascular device for adults. For a patient with no contraindications, what antiseptic should the IP suggest?
Options:
Chlorhexidine
Povidone-iodine
Alcohol
Antibiotic ointment
Answer:
AExplanation:
The selection of an appropriate antiseptic for the insertion of an intravascular device (e.g., peripheral or central venous catheters) is a critical infection prevention measure to reduce the risk of catheter-related bloodstream infections (CRBSIs). The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes evidence-based practices in the "Prevention and Control of Infectious Diseases" domain, which includes adhering to guidelines for aseptic technique during invasive procedures. The Centers for Disease Control and Prevention (CDC) provides specific recommendations for skin antisepsis, as outlined in the "Guidelines for the Prevention of Intravascular Catheter-Related Infections" (2017).
Option A, chlorhexidine, is the preferred antiseptic for skin preparation prior to intravascular device insertion in adults with no contraindications. Chlorhexidine, particularly in a 2% chlorhexidine gluconate (CHG) with 70% isopropyl alcohol solution, is recommended by the CDC due to its broad-spectrum antimicrobial activity, residual effect (which continues to kill bacteria after application), and superior efficacy compared to other agents in reducing CRBSI rates. Studies cited in the CDC guidelines demonstrate that chlorhexidine-based preparations significantly lower infection rates compared to povidone-iodine or alcohol alone, making it the gold standard for this procedure when tolerated by the patient.
Option B, povidone-iodine, is an alternative antiseptic that can be used for skin preparation. It is effective against a wide range of microorganisms and is often used when chlorhexidine is contraindicated (e.g., in patients with chlorhexidine allergy). However, its efficacy is less persistent than chlorhexidine, and it requires longer drying time, which can be a limitation in busy clinical settings. The CDC considers povidone-iodine a second-line option unless chlorhexidine is unavailable or unsuitable. Option C, alcohol (e.g., 70% isopropyl or ethyl alcohol), has rapid bactericidal activity but lacks a residual effect, making it less effective for prolonged protection during catheter dwell time. It is often used as a component of chlorhexidine-alcohol combinations but is not recommended as a standalone antiseptic for intravascular device insertion. Option D, antibiotic ointment, is not appropriate for skin preparation during insertion. Antibiotic ointments (e.g., bacitracin or mupirocin) are sometimes applied to catheter sites post-insertion to prevent infection, but their use is discouraged by the CDC due to the risk of promoting antibiotic resistance and fungal infections, and they are not classified as antiseptics for initial skin antisepsis.
The CBIC Practice Analysis (2022) supports the adoption of CDC-recommended practices, and the 2017 CDC guidelines explicitly state that chlorhexidine-based preparations with alcohol should be used for skin antisepsis unless contraindicated. For a patient with no contraindications, the infection preventionist should suggest chlorhexidine to optimize patient safety and align with best practices.
An infection preventionist is notified of a patient with Gram negative diplococci from a cerebral spinal fluid specimen. The patient was intubated during ambulance transport and intravenous lines are placed after arrival to the Emergency Department (ED). The patient was immediately placed in Droplet Precautions upon admission to the ED. Which of the following statements is true regarding the need for evaluating exposure to communicable illness?
Options:
Follow-up evaluation is not required for this laboratory finding.
ED personnel should be evaluated for possible exposure.
Ambulance personnel should be evaluated for possible exposure.
Follow-up evaluation is not necessary as the appropriate precautions were promptly instituted.
Answer:
CExplanation:
The correct answer is C, "Ambulance personnel should be evaluated for possible exposure," as this statement is true regarding the need for evaluating exposure to communicable illness. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, the presence of Gram negative diplococci in a cerebral spinal fluid (CSF) specimen is suggestive of a serious bacterial infection, most likely Neisseria meningitidis, which causes meningococcal disease. This condition is highly contagious and can be transmitted through respiratory droplets or direct contact with respiratory secretions, particularly during procedures like intubation (CBIC Practice Analysis, 2022, Domain I: Identification of Infectious Disease Processes, Competency 1.1 - Identify infectious disease processes). The patient was intubated during ambulance transport, creating a potential aerosol-generating procedure (AGP) that could have exposed ambulance personnel to infectious droplets before Droplet Precautions were instituted upon arrival at the Emergency Department (ED). Therefore, evaluating ambulance personnel for possible exposure is necessary to assess their risk and determine if post-exposure prophylaxis (e.g., antibiotics) or monitoring is required.
Option A (follow-up evaluation is not required for this laboratory finding) is incorrect because the identification of Gram negative diplococci in CSF is a critical finding that warrants investigation due to the potential for meningococcal disease, a reportable and transmissible condition. Option B (ED personnel should be evaluated for possible exposure) is less applicable since the patient was immediately placed in Droplet Precautions upon ED admission, minimizing exposure risk to ED staff after that point, though it could be considered if exposure occurred before precautions were fully implemented. Option D (follow-up evaluation is not necessary as the appropriate precautions were promptly instituted) is inaccurate because the prompt institution of Droplet Precautions in the ED does not retroactively address the exposure risk during ambulance transport, where precautions were not in place.
The focus on evaluating ambulance personnel aligns with CBIC’s emphasis on identifying and mitigating transmission risks associated with communicable diseases, particularly in high-risk settings like ambulance transport (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). This step is supported by CDC guidelines, which recommend exposure evaluation and prophylaxis for close contacts of meningococcal disease cases (CDC Meningococcal Disease Management, 2021).
Steam sterilization should be validated with which of the following organisms?
Options:
Geobacillus stearothermophilus
Staphylococcus aureus
Bacillus anthracis
Bacillus atrophaeus
Answer:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) clearly states that steam sterilization (moist heat sterilization) must be validated using biological indicators containing Geobacillus stearothermophilus spores. This organism is selected because its spores are highly resistant to moist heat, making them an ideal challenge organism for assessing the effectiveness of steam sterilization processes.
Biological indicators are used to confirm that sterilization conditions—such as temperature, pressure, and exposure time—are sufficient to achieve microbial inactivation. Geobacillus stearothermophilus thrives at high temperatures and demonstrates strong resistance to steam, so if these spores are destroyed, it provides high confidence that other less-resistant microorganisms, including bacteria, viruses, and fungi, have also been eliminated.
The other options are incorrect for steam sterilization validation. Staphylococcus aureus is a vegetative bacterium and is far less resistant than bacterial spores. Bacillus anthracis is not used as a biological indicator due to safety concerns and lack of standardization. Bacillus atrophaeus is used as the biological indicator for dry heat and ethylene oxide sterilization, not steam.
Understanding which biological indicators correspond to specific sterilization modalities is a high-yield topic on the CIC® exam and is essential for ensuring compliance with evidence-based sterilization and disinfection standards.
=======
The intensive care unit has noted an increase in patients with ventilator-associated events (VAEs). Which of the following may be contributing to the increase in these events?
Options:
Supine position during transport
Daily sedation vacation
Daily weaning assessment
Daily oral care with chlorhexidine
Answer:
AExplanation:
Ventilator-associated events (VAEs) are complications that occur in patients receiving mechanical ventilation and include conditions such as ventilator-associated pneumonia (VAP), pulmonary edema, and atelectasis. The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that patient positioning plays a critical role in preventing aspiration and subsequent respiratory complications in mechanically ventilated patients.
Maintaining patients in a supine position, particularly during transport, increases the risk of aspiration of gastric contents and oropharyngeal secretions. Aspiration is a well-recognized contributing factor to the development of VAEs because it can lead to infection, inflammation, and worsening oxygenation. The Study Guide recommends maintaining the head of the bed elevated (generally 30–45 degrees) whenever feasible, including during care activities and transport, to reduce aspiration risk.
The other options listed—daily sedation vacation, daily weaning assessment, and daily oral care with chlorhexidine—are evidence-based prevention strategies that are part of ventilator care bundles. These interventions are designed to reduce the duration of mechanical ventilation, improve pulmonary function, and decrease microbial colonization, all of which lower the risk of VAEs rather than contribute to them.
Therefore, supine positioning during transport is the most likely factor contributing to an increase in ventilator-associated events and represents a deviation from recommended infection prevention practices.
Working with public health agencies to collect and analyze indicators that might signal an increase in community illness is an example of which type of surveillance?
Options:
Passive
Active
Syndromic
Targeted
Answer:
CExplanation:
Surveillance is a critical tool in infection prevention and control, used to monitor disease trends and guide public health responses. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes the "Surveillance and Epidemiologic Investigation" domain, which aligns with the Centers for Disease Control and Prevention (CDC) "Principles of Epidemiology in Public Health Practice" (3rd Edition, 2012). The question describes a process of collecting and analyzing indicators to signal an increase in community illness, requiring identification of the appropriate surveillance type among the options provided.
Option C, "Syndromic," is the correct answer. Syndromic surveillance involves monitoring non-specific health indicators or symptoms (e.g., fever, respiratory complaints, or gastrointestinal issues) that may precede a formal diagnosis, aiming to detect potential outbreaks or increases in community illness early. The CDC defines syndromic surveillance as the real-time or near-real-time collection, analysis, and interpretation of health-related data to provide actionable information, often in collaboration with public health agencies. This approach uses data from sources like emergency department visits, over-the-counter medication sales, or absenteeism reports to identify trends before laboratory confirmation, making it well-suited to the described scenario of signaling community illness increases.
Option A, "Passive," involves healthcare providers or laboratories reporting cases to public health authorities on a voluntary or mandatory basis without active prompting (e.g., routine notifiable disease reporting). While passive surveillance contributes to baseline data, it is less proactive and not specifically designed to signal early increases in illness, making it less fitting. Option B, "Active," entails public health officials actively seeking data from healthcare facilities or providers (e.g., calling to confirm cases during an outbreak). This is more resource-intensive and typically used for specific investigations rather than ongoing community trend monitoring, which aligns better with syndromic methods. Option D, "Targeted," refers to surveillance focused on a specific population, disease, or event (e.g., monitoring TB in a high-risk group). The scenario’s broad focus on community illness indicators does not suggest a targeted approach.
The CBIC Practice Analysis (2022) and CDC guidelines highlight syndromic surveillance as a key strategy for early detection of community-wide health threats, often involving collaboration with public health agencies. Option C best matches the described activity of analyzing indicators to signal illness increases, making it the correct choice.
Which of the following should be included when designing a data collection form for surveillance?
Options:
Denominator information
Only the information needed
As much information as possible
Medication history
Answer:
AExplanation:
The Certification Study Guide (6th edition) emphasizes that effective surveillance depends on the ability to calculate rates, not just counts. To calculate any infection rate, both a numerator (number of infection events) and a denominator (population at risk or time at risk) are required. Therefore, inclusion of denominator information is essential when designing a data collection form for surveillance.
Denominator data may include patient days, device days (e.g., central line days, ventilator days), number of procedures, or number of admissions—depending on the surveillance objective. Without denominator data, infection preventionists cannot calculate standardized rates, compare trends over time, or benchmark against national databases. The study guide clearly states that surveillance systems lacking denominator data produce incomplete and potentially misleading results.
The other options are either vague or inappropriate. While data collection forms should avoid unnecessary information, simply stating “only the information needed” does not address the critical requirement for denominator data. Collecting “as much information as possible” is discouraged because it increases workload, reduces data quality, and may compromise sustainability of surveillance programs. Medication history is not routinely required for most surveillance activities unless it is directly related to the infection being studied.
This question reflects a fundamental CIC exam principle: surveillance must be designed to support valid rate calculation and analysis. Including denominator information ensures that collected data are meaningful, actionable, and aligned with evidence-based infection prevention practices.
Each item or package that is prepared for sterilization should be labeled with the
Options:
storage location.
type of sterilization process.
sterilizer identification number or code.
cleaning method (e.g., mechanical or manual).
Answer:
CExplanation:
The correct answer is C, "sterilizer identification number or code," as this is the essential information that each item or package prepared for sterilization should be labeled with. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, proper labeling of sterilized items is a critical component of infection prevention and control to ensure traceability and verify the sterilization process. The sterilizer identification number or code links the item to a specific sterilization cycle, allowing the infection preventionist (IP) and sterile processing staff to track the equipment used, confirm compliance with standards (e.g., AAMI ST79), and facilitate recall or investigation if issues arise (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.3 - Ensure safe reprocessing of medical equipment). This labeling ensures that the sterility of the item can be assured and documented, protecting patient safety by preventing the use of inadequately processed items.
Option A (storage location) is important for inventory management but is not directly related to the sterilization process itself and does not provide evidence of the sterilization event. Option B (type of sterilization process) indicates the method (e.g., steam, ethylene oxide), which is useful but less critical than the sterilizer identification, as the process type alone does not confirm the specific cycle or equipment used. Option D (cleaning method, e.g., mechanical or manual) is a preliminary step in reprocessing, but it is not required on the sterilization label, as the focus shifts to sterilization verification once the item is prepared.
The requirement for a sterilizer identification number or code aligns with CBIC’s emphasis on maintaining rigorous tracking and quality assurance in the reprocessing of medical devices, ensuring accountability and adherence to best practices (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). This practice is mandated by standards such as AAMI ST79 to support effective infection control in healthcare settings.
A patient with pertussis can be removed from Droplet Precautions after
Options:
direct fluorescent antibody and/or culture are negative.
five days of appropriate antibiotic therapy.
the patient has been given pertussis vaccine.
the paroxysmal stage has ended.
Answer:
BExplanation:
A patient with pertussis (whooping cough) should remain on Droplet Precautions to prevent transmission. According to APIC guidelines, patients with pertussis can be removed from Droplet Precautions after completing at least five days of appropriate antimicrobial therapy and showing clinical improvement.
Why the Other Options Are Incorrect?
A. Direct fluorescent antibody and/or culture are negative – Laboratory results may not always detect pertussis early, and false negatives can occur.
C. The patient has been given pertussis vaccine – The vaccine prevents but does not treat pertussis, and it does not shorten the period of contagiousness.
D. The paroxysmal stage has ended – The paroxysmal stage (severe coughing fits) can last weeks, but infectiousness decreases with antibiotics.
CBIC Infection Control Reference
According to APIC guidelines, Droplet Precautions should continue until the patient has received at least five days of antimicrobial therapy.
Assume the mean age of onset for patients with tuberculosis (TB) is 62 years, with one standard deviation of 5 years, and the age of onset follows a normal distribution. What is the percentage of patients expected to have the age of onset ranging from 57 to 67 years?
Options:
34%
68%
95%
99%
Answer:
BExplanation:
To determine the percentage of patients with an age of onset ranging from 57 to 67 years, we need to apply the properties of a normal distribution. In a normal distribution, the mean represents the central point, and the standard deviation defines the spread of the data. Here, the mean age of onset is 62 years, and the standard deviation is 5 years. The range of 57 to 67 years corresponds to one standard deviation below the mean (62 - 5 = 57) to one standard deviation above the mean (62 + 5 = 67).
In a normal distribution, approximately 68% of the data falls within one standard deviation of the mean (i.e., between μ - σ and μ + σ, where μ is the mean and σ is the standard deviation). This is a well-established statistical principle, often referred to as the 68-95-99.7 rule (or empirical rule) in statistics. Specifically, 34% of the data lies between the mean and one standard deviation above the mean, and another 34% lies between the mean and one standard deviation below the mean, totaling 68% for the range spanning one standard deviation on both sides of the mean.
Let’s verify this:
The lower bound (57 years) is exactly one standard deviation below the mean (62 - 5 = 57).
The upper bound (67 years) is exactly one standard deviation above the mean (62 + 5 = 67).
Thus, the range from 57 to 67 years encompasses the middle 68% of the distribution.
Option A (34%) represents the percentage of patients within one standard deviation on only one side of the mean (e.g., 62 to 67 or 57 to 62), not the full range. Option C (95%) corresponds to approximately two standard deviations from the mean (62 ± 10 years, or 52 to 72 years), which is wider than the given range. Option D (99%) aligns with approximately three standard deviations (62 ± 15 years, or 47 to 77 years), which is even broader. Since the question specifies a range of one standard deviation on either side of the mean, the correct answer is 68%, corresponding to Option B.
In infection control, understanding the distribution of disease onset ages can help infection preventionists identify at-risk populations and allocate resources effectively, aligning with the CBIC’s focus on surveillance and data analysis (CBIC Practice Analysis, 2022). While the CBIC does not directly address statistical calculations in its core documents, the application of normal distribution principles is a standard epidemiological tool endorsed in public health guidelines, which inform CBIC practices.
The BEST roommate selection for a patient with active shingles would be a patient who has had
Options:
varicella vaccine.
treatment with acyclovir
a history of herpes simplex.
varicclla zoster immunoglobulin
Answer:
AExplanation:
A patient with active shingles (herpes zoster) is contagious to individuals who have never had varicella (chickenpox) or the varicella vaccine. The best roommate selection is someone who has received the varicella vaccine, as they are considered immune and not at risk for contracting the virus.
Why the Other Options Are Incorrect?
B. Treatment with acyclovir – Acyclovir treats herpes zoster but does not prevent transmission to others.
C. A history of herpes simplex – Prior herpes simplex virus (HSV) infection does not confer immunity to varicella-zoster virus (VZV).
D. Varicella zoster immunoglobulin (VZIG) – VZIG provides temporary immunity but does not offer long-term protection like the vaccine.
CBIC Infection Control Reference
APIC guidelines recommend placing patients with active shingles in a room with individuals immune to varicella, such as those vaccinated.
During an outbreak of ventilator-associated pneumonia (VAP), the infection preventionist should FIRST:
Options:
Review adherence to ventilator bundle elements.
Implement preemptive antibiotic therapy in all ventilated patients.
Isolate all ventilated patients in negative pressure rooms.
Perform bacterial cultures from ventilator circuits.
Answer:
AExplanation:
Reviewing compliance with VAP prevention bundles (e.g., head-of-bed elevation, oral care, sedation breaks) is the first step in outbreak control.
Preemptive antibiotics (B) are not recommended due to antibiotic resistance risks.
Negative pressure rooms (C) are not required for VAP.
Ventilator circuit cultures (D) do not guide patient management.
CBIC Infection Control References:
APIC Text, "VAP Prevention Measures," Chapter 11.
To understand how their hospital-acquired infection rates compare to other health care settings, an infection preventionist (IP) plans to use benchmarking.
Which of the following criteria is important to ensure accurate benchmarking of surveillance data?
Options:
Data collectors are trained on how to collect data
Collecting data on a small population lo ensure accuracy of data collection
Denominator rates are selected based on an organizational risk assessment
Using case definitions that are adjusted for the patient population being studied
Answer:
DExplanation:
Benchmarking compares infection rates across healthcare facilities. For accurate benchmarking, case definitions must be standardized and adjusted for patient demographics, severity of illness, and other risk factors.
Why the Other Options Are Incorrect?
A. Data collectors are trained on how to collect data – Training is necessary, but it does not directly ensure comparability between facilities.
B. Collecting data on a small population – A larger sample size increases accuracy and reliability in benchmarking.
C. Denominator rates selected based on an organizational risk assessment – Risk assessment is important, but standardized case definitions are critical for comparison.
CBIC Infection Control Reference
According to APIC, accurate benchmarking relies on using standardized case definitions that account for differences in patient populations.
A patient with shortness of breath and a history of a tuberculin skin test (TST) of 15 mm induration was admitted to a semi-private room. The infection preventionist's FIRST action should be to
Options:
contact the roommate's physician to initiate TST.
review the patient's medical record to determine the likelihood of pulmonary tuberculosis (TB).
report the findings to the Employee Health Department to initiate exposure follow-up of hospital staff.
transfer the patient to an airborne infection isolation room and initiate appropriate isolation for tuberculosis (TB).
Answer:
BExplanation:
Before initiating airborne precautions, the infection preventionist must first confirm the clinical suspicion of active TB.
Step-by-Step Justification:
Confirming Active TB:
A positive tuberculin skin test (TST) alone does not indicate active disease.
A review of chest X-ray, symptoms, and risk factors is needed.
Medical Record Review:
Past TB history, imaging, and sputum testing are key to diagnosis.
Not all TST-positive patients require isolation.
Why Other Options Are Incorrect:
A. Contact the roommate's physician to initiate TST: Premature, as no confirmation of active TB exists yet.
C. Report findings to Employee Health for staff follow-up: Should occur only after TB confirmation.
D. Transfer to airborne isolation immediately: Airborne isolation is necessary only if active TB is suspected based on clinical findings.
CBIC Infection Control References:
The annual report for Infection Prevention shows a dramatic decrease in urinary catheter days, a decrease in the catheter utilization ratio, and a slight decrease in the number of catheter-associated urinary tract infections (CAUTIs). The report does not show an increase in the overall rate of CAUTI. How would the infection preventionist explain this to the administration?
Options:
The rate is incorrect and needs to be recalculated.
The rate may be higher if the denominator is very small.
The rate is not affected by the number of catheter days.
Decreasing catheter days will not have an effect on decreasing CAUTI.
Answer:
BExplanation:
The correct answer is B, "The rate may be higher if the denominator is very small," as this provides the most plausible explanation for the observed data in the annual report. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, the CAUTI rate is calculated as the number of CAUTIs per 1,000 catheter days, where catheter days serve as the denominator. The report indicates a dramatic decrease in urinary catheter days and a slight decrease in the number of CAUTIs, yet the overall CAUTI rate has not increased. This discrepancy can occur if the denominator (catheter days) becomes very small, which can inflate or destabilize the rate, potentially masking an actual increase in the infection risk per catheter day (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.2 - Analyze surveillance data). A smaller denominator amplifies the impact of even a slight change in the number of infections, suggesting that the rate may be higher than expected or less reliable, necessitating further investigation.
Option A (the rate is incorrect and needs to be recalculated) assumes an error in the calculation without evidence, which is less specific than the denominator effect explanation. Option C (the rate is not affected by the number of catheter days) is incorrect because the CAUTI rate is directly influenced by the number of catheter days as the denominator; a decrease in catheter days should typically lower the rate if infections decrease proportionally, but the lack of an increase here suggests a calculation or interpretation issue. Option D (decreasing catheter days will not have an effect on decreasing CAUTI) contradicts evidence-based practice, as reducing catheter days is a proven strategy to lower CAUTI incidence, though the rate’s stability here indicates a potential statistical artifact.
The explanation focusing on the denominator aligns with CBIC’s emphasis on accurate surveillance and data analysis to guide infection prevention strategies, allowing the infection preventionist to advise administration on the need to review data trends or adjust monitoring methods (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.5 - Use data to guide infection prevention and control strategies). This insight can prompt a deeper analysis to ensure the CAUTI rate reflects true infection risk.
How can infection preventionists BEST educate on a new infection prevention protocol for adoption across different departments within an organization?
Options:
Relate relevance of each department’s role using scenarios.
Utilize a passive learning method to accommodate for diversity.
Assign reading and review of protocol with manager sign-off.
Tie protocol compliance metric to annual performance review.
Answer:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that effective education for adult learners is most successful when it is relevant, interactive, and role-specific. Relating the new infection prevention protocol to each department’s responsibilities using realistic scenarios is the most effective educational strategy for organization-wide adoption.
Scenario-based education is an active learning method, which engages participants in problem-solving and application of knowledge rather than passive receipt of information. By tailoring scenarios to departmental workflows—such as nursing, environmental services, laboratory, or ancillary departments—staff can clearly understand how the protocol affects their daily practice and how their actions contribute to infection prevention outcomes. This approach improves comprehension, retention, and compliance.
Option B is incorrect because passive learning methods (e.g., lectures or handouts alone) are less effective for behavior change and adult learning. Option C relies on administrative acknowledgment rather than understanding and does not ensure competency or consistent application. Option D may support accountability but does not educate staff or build understanding during initial implementation.
The Study Guide stresses that infection preventionists must act as educators and change agents, adapting teaching strategies to diverse audiences. Using scenario-based, department-specific education aligns with adult learning principles, promotes engagement, and facilitates sustainable practice change—making it the best approach and a key concept for the CIC® exam.
==========
The MOST common route of infection for healthcare-associated (HA) pneumonia is:
Options:
Aspiration of bacteria from the oropharynx
Person-to-person spread from healthcare personnel’s (HCP) hands
Contamination from small-volume nebulizers
Droplet inhalation from large-volume humidifiers
Answer:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) identifies aspiration of bacteria from the oropharynx as the most common route of infection for healthcare-associated pneumonia, including hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP). In hospitalized patients—especially those who are critically ill, sedated, intubated, or have impaired consciousness—the normal defense mechanisms that prevent aspiration are compromised.
Colonization of the oropharynx with pathogenic organisms occurs rapidly in hospitalized patients due to factors such as antibiotic exposure, underlying illness, poor oral hygiene, and use of invasive devices. Microaspiration of contaminated oral and gastric secretions into the lower respiratory tract is a frequent event and represents the primary mechanism by which pathogens reach the lungs. This risk is significantly increased in patients receiving mechanical ventilation or those positioned supine.
The other options represent less common routes. Transmission from healthcare personnel hands (Option B) contributes indirectly by facilitating colonization but is not the primary route of pneumonia development. Contaminated nebulizers (Option C) and humidifiers (Option D) have been associated with outbreaks but are now uncommon causes due to improved equipment design and maintenance practices.
For CIC® exam preparation, it is essential to recognize that preventive strategies for HA pneumonia focus heavily on reducing aspiration risk, including head-of-bed elevation, oral care protocols, and minimizing sedation—directly addressing the most common route of infection.
A nurse claims to have acquired hepatitis A virus infection as the result of occupational exposure. The source patient had an admitting diagnosis of viral hepatitis. Further investigation of this incident reveals a 5-day interval between exposure and onset of symptoms in the nurse. The patient has immunoglobulin G antibodies to hepatitis A. From the evidence, the infection preventionist may correctly conclude which of the following?
Options:
The nurse should be given hepatitis A virus immunoglobulin.
The evidence at this time fails to support the nurse's claim.
The patient has serologic evidence of recent hepatitis A viral infection.
The 5-day incubation period is consistent with hepatitis A virus transmission.
Answer:
BExplanation:
The infection preventionist’s (IP) best conclusion, based on the provided evidence, is that the evidence at this time fails to support the nurse's claim of acquiring hepatitis A virus (HAV) infection through occupational exposure. This conclusion is grounded in the clinical and epidemiological understanding of HAV, as aligned with the Certification Board of Infection Control and Epidemiology (CBIC) guidelines. Hepatitis A typically has an incubation period ranging from 15 to 50 days, with an average of approximately 28-30 days, following exposure to the virus (CBIC Practice Analysis, 2022, Domain I: Identification of Infectious Disease Processes, Competency 1.3 - Apply principles of epidemiology). The reported 5-day interval between exposure and symptom onset in the nurse is significantly shorter than the expected incubation period, making it inconsistent with HAV transmission. Additionally, the presence of immunoglobulin G (IgG) antibodies in the source patient indicates past exposure or immunity to HAV, rather than an active or recent infection, which would typically be associated with immunoglobulin M (IgM) antibodies during the acute phase.
Option A (the nurse should be given hepatitis A virus immunoglobulin) is not supported because post-exposure prophylaxis with HAV immunoglobulin is recommended only within 14 days of exposure to a confirmed case with active infection, and the evidence here does not confirm a recent exposure or active case. Option C (the patient has serologic evidence of recent hepatitis A viral infection) is incorrect because IgG antibodies signify past infection or immunity, not a recent infection, which would require IgM antibodies. Option D (the 5-day incubation period is consistent with hepatitis A virus transmission) is inaccurate due to the mismatch with the known incubation period of HAV.
The IP’s role includes critically evaluating epidemiological data to determine the likelihood of transmission events. The discrepancy in the incubation period and the serologic status of the patient suggest that the nurse’s claim may not be substantiated by the current evidence, necessitating further investigation rather than immediate intervention or acceptance of the claim. This aligns with CBIC’s emphasis on accurate identification and investigation of infectious disease processes (CBIC Practice Analysis, 2022, Domain I: Identification of Infectious Disease Processes, Competency 1.2 - Investigate suspected outbreaks or exposures).
A patient with a non-crusted rash has boon diagnosed with Sarcoptes scabiei. The patient is treated with 5% permethrin and precautions are started. The precautions can be stopped
Options:
when the treatment cream is applied
when the bed linen is changed
24 hours after effective treatment
24 hours after the second treatment
Answer:
CExplanation:
For Sarcoptes scabiei (scabies), Contact Precautions should remain in place until 24 hours after effective treatment has been completed. The first-line treatment is 5% permethrin cream, which is applied to the entire body and left on for 8–14 hours before being washed off.
Why the Other Options Are Incorrect?
A. When the treatment cream is applied – The mite is still present and infectious until treatment has fully taken effect.
B. When the bed linen is changed – While changing linens is necessary, it does not indicate that the infestation has cleared.
D. 24 hours after the second treatment – Most cases require only one treatment with permethrin, though severe cases may need a second dose after a week.
CBIC Infection Control Reference
According to APIC guidelines, Contact Precautions can be discontinued 24 hours after effective treatment has been administered.
In the Preparedness and Response Framework for Influenza Pandemics, intervals are used to describe an influenza pandemic progression. The interval “Deceleration of the Pandemic Wave” is characterized by:
Options:
Subject matter experts’ judgment of the potential implications for human health.
Identification of novel influenza A in humans or animals anywhere in the world.
Low pandemic influenza activity but continued possible outbreaks.
Consistently decreasing rate of pandemic influenza cases.
Answer:
DExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) describes the Preparedness and Response Framework for Influenza Pandemics as a structured model that divides a pandemic into distinct intervals to guide public health and healthcare response activities. These intervals include investigation, recognition, initiation, acceleration, deceleration, and preparation for future waves.
The Deceleration of the Pandemic Wave interval is defined by a consistent and sustained decrease in the number of new pandemic influenza cases, hospitalizations, and deaths. This decline reflects the impact of mitigation strategies such as vaccination campaigns, antiviral use, nonpharmaceutical interventions, and the development of population immunity. Although transmission is decreasing, healthcare systems are advised to remain vigilant, as localized transmission may still occur.
Option A describes activities associated with the Investigation Interval, when experts assess the potential public health implications of a novel virus. Option B corresponds to the Recognition Interval, marked by identification of a novel influenza A virus. Option C aligns more closely with the Preparation for Future Waves Interval, when overall activity is low but the risk of resurgence remains.
Understanding these distinctions is critical for infection preventionists, as response priorities shift during each interval. During deceleration, focus transitions from surge response to recovery planning, evaluation of response effectiveness, and preparation for potential subsequent waves—key concepts emphasized in the CIC® exam.
==========
`
In order to ensure accurate calculation of central line days, which of the following is TRUE?
Options:
Tunneled catheters and ports should be excluded.
A catheter should be in place for longer than 24 hours to be counted.
A patient with more than one device is counted as 1 device day.
Peripheral lines should be included in ICU data.
Answer:
CExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) follows the standardized surveillance methodology used for calculating central line days, which is essential for accurate reporting of central line–associated bloodstream infection (CLABSI) rates. A central line day is counted for each patient who has one or more central lines in place at the time of the daily count, regardless of the number of central lines present.
Therefore, if a patient has more than one central line, the patient is still counted as one central line day, making option C the correct statement. This approach ensures consistency and comparability of CLABSI rates across units and facilities.
Option A is incorrect because tunneled central venous catheters and implanted ports are included in central line counts if they meet the definition of a central line. Option B is incorrect because a central line is counted on any day it is present, even if it has been in place for less than 24 hours. Option D is incorrect because peripheral intravenous lines are not central lines and must never be included in central line day counts.
Accurate calculation of device days is a foundational surveillance competency for infection preventionists. Understanding these definitions is critical for valid CLABSI rate calculation, benchmarking, and performance improvement and is a frequently tested concept on the CIC® exam.
The Sterile Processing Deportment alerts an infection preventionist that a load of surgical Instruments sterilized with high temperature steam:moist heat needs to be recalled. Which of the following Is the MOST likely reason for the recall?
Options:
Failure of the biological Indicator Bacillus subtilts
Failure of the biological Indicator Geobaciltus stearothermophilus
Placement of the biological Indicator on the bottom shelf over the d*an
Incorrect placement of the instruments In the tray
Answer:
BExplanation:
The most likely reason for the recall of a steam-sterilized load is the failure of the biological indicator (BI), specifically Geobacillus stearothermophilus, which is used to monitor high-temperature steam (moist heat) sterilization processes. This organism is the biological indicator of choice because it has high resistance to moist heat and thus serves as a reliable marker for sterilization efficacy.
The APIC Text and AAMI ST79 guidelines confirm that Geobacillus stearothermophilus is used for steam sterilization and that a failed BI indicates a failure in the sterilization process, which requires immediate action, including recalling all items sterilized since the last negative BI and reprocessing them. This is a crucial aspect of ensuring patient safety and preventing the use of potentially non-sterile surgical instruments.
According to the APIC Text:
"BIs are the only process indicators that directly monitor the lethality of a given sterilization process. [...] Geobacillus stearothermophilus spores are used to monitor steam sterilization..."
The CIC Study Guide (6th ed.) also specifies that:
"Evidence of sterilization failures (e.g., positive biological indicators) is the most common reason for a recall."
Additionally, it is noted:
“With steam sterilization, the instrument load does not need to be recalled for a single positive biological indicator test, with the exception of implantable objects.”
However, multiple positive BIs or BI failure confirmation does require a recall.
The incorrect options explained:
A. Bacillus subtilis – This is not used in steam sterilization but rather in dry heat or EO processes.
C. Placement of the biological indicator on the bottom shelf over the drain – While incorrect placement can lead to test failure, the recall is prompted by BI failure, not just placement.
D. Incorrect placement of instruments – This can cause sterilization failure but is not the direct trigger for a recall unless it leads to a failed BI.
Which of the following blood-drawing methods is considered to be a needle-safe practice?
Options:
Use a syringe with a needle attached.
Shielded needles for vacuum-tube phlebotomy sets.
Remove contaminated needles from blood collection sets.
Inject blood into vacuum tubes using conventional syringes.
Answer:
BExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) identifies engineered sharps injury prevention devices (ESIPDs) as the cornerstone of needle-safe practices during blood collection. Shielded needles used with vacuum-tube phlebotomy systems are specifically designed to reduce the risk of needlestick injuries by incorporating a built-in safety mechanism that covers or retracts the needle immediately after use.
Vacuum-tube systems with shielded needles allow blood to flow directly into collection tubes without the need for needle removal or blood transfer, thereby minimizing handling of sharps. Once blood collection is complete, the safety feature is activated—often automatically or with a single-handed technique—significantly reducing exposure risk to healthcare personnel. The Study Guide emphasizes that these devices meet regulatory expectations under the Needlestick Safety and Prevention Act and should be used whenever feasible.
The other options are unsafe practices. Using syringes with attached needles (Option A) increases risk during transfer and disposal. Removing contaminated needles from collection sets (Option C) is explicitly prohibited due to high injury risk. Injecting blood into vacuum tubes using conventional syringes (Option D) requires manipulating exposed needles and increases the likelihood of splashes and sharps injuries.
For CIC® exam preparation, it is essential to recognize that needle-safe blood collection relies on safety-engineered devices, with shielded vacuum-tube phlebotomy needles representing best practice for preventing occupational exposures.
Endemic infection rate refers to
Options:
Disease that overwhelms the usual healthcare system.
The usual presence of a disease in a specific population or geographical area.
An outbreak of disease much greater than expected in a specific population or group.
The occurrence of more cases of a disease than expected in a given area or among a specific group.
Answer:
BExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) defines endemic infection rate as the constant or usual presence of a disease within a specific population, geographic area, or healthcare setting. An endemic level represents the baseline or expected frequency of disease occurrence over time, allowing infection preventionists to distinguish normal disease patterns from unusual increases that may signal outbreaks or epidemics.
Option B accurately reflects this definition by describing the expected and stable presence of a disease within a defined population or location. Endemic infections may persist at low or predictable levels and do not necessarily indicate a failure of infection prevention practices. Examples include seasonal influenza in the community or baseline rates of certain healthcare-associated infections within a facility.
Option A refers to a pandemic or healthcare system overload, not endemic disease. Options C and D describe outbreaks or epidemics, which involve a sudden increase in cases above the expected endemic level. These terms imply deviation from baseline and require investigation and intervention.
Understanding endemic rates is critical for infection prevention and surveillance because they provide the comparison point for identifying trends, clusters, and outbreaks. Surveillance data are interpreted against endemic baselines to determine whether changes reflect random variation or meaningful increases requiring action.
For the CIC® exam, recognizing epidemiologic terminology is essential. Endemic infection rate specifically refers to the usual or expected presence of disease, making option B the correct answer.
Major construction and renovations are planned for a hospital’s operating suite, and a meeting is scheduled to plan for construction activities. Aside from the infection preventionist, and representatives from environmental services and engineering, who else should be included in these planning conversations?
Options:
Operating room nurse manager
Chief operating officer
Plumbing supervisor
Director of public relations
Answer:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that multidisciplinary collaboration is essential when planning construction or renovation projects in patient care areas, especially high-risk locations such as operating suites. In addition to infection prevention, environmental services, and engineering, the operating room nurse manager must be actively involved in construction planning discussions.
The operating room nurse manager represents frontline clinical operations and has direct knowledge of surgical workflows, patient movement, sterile processing needs, case scheduling, and staff practices. Their involvement ensures that construction activities are coordinated to minimize disruption to patient care, maintain sterile environments, and reduce infection risks associated with dust, airflow changes, and traffic patterns. The nurse manager also plays a key role in communicating construction-related precautions and practice changes to surgical staff.
While senior leadership (Option B) may provide oversight, they are not typically involved in detailed infection control planning. The plumbing supervisor (Option C) may be consulted for specific infrastructure issues but does not represent clinical operations. The director of public relations (Option D) is not relevant to construction-related infection risk planning.
The Study Guide highlights that ICRA planning must include clinical leadership from affected areas to ensure that infection prevention measures are practical, effective, and consistently implemented. Including the operating room nurse manager is therefore essential for safe construction planning and is a frequently tested CIC® exam concept.
==========
A suspected measles case has been identified in an outpatient clinic without an airborne infection isolation room (AIIR). Which of the following is the BEST course of action?
Options:
Patient should be sent home
Staff should don a respirator, gown, and face shield.
Patient should be offered the Measles. Mumps, Rubella (MMR) vaccine
Patient should be masked and placed in a private room with door closed.
Answer:
DExplanation:
Measles is a highly contagious airborne disease, and the best immediate action in an outpatient clinic without an Airborne Infection Isolation Room (AIIR) is to mask the patient and isolate them in a private room with the door closed.
Why the Other Options Are Incorrect?
A. Patient should be sent home – While home isolation may be necessary, sending the patient home without proper precautions increases exposure risk.
B. Staff should don a respirator, gown, and face shield – While N95 respirators are necessary for staff, this does not address patient containment.
C. Patient should be offered the MMR vaccine – The vaccine does not treat active measles infection and should be given only as post-exposure prophylaxis to susceptible contacts.
CBIC Infection Control Reference
Measles cases in outpatient settings require immediate airborne precautions to prevent transmission.
A hospital is experiencing an increase in multidrug-resistant Acinetobacter baumannii infections in the intensive care unit (ICU). The infection preventionist's FIRST action should be to:
Options:
Implement universal contact precautions for all ICU patients.
Conduct an epidemiologic investigation to identify potential sources.
Perform environmental sampling to detect Acinetobacter on surfaces.
Initiate decolonization protocols for all ICU patients.
Answer:
BExplanation:
Epidemiologic Investigation:
The first step in an outbreak response is to characterize cases by person, place, and time.
Identifying common exposures (e.g., ventilators, catheters, or contaminated surfaces) helps determine the source.
Why Other Options Are Incorrect:
A. Universal contact precautions: Premature; precautions should be tailored based on transmission patterns.
C. Environmental sampling: Should be done after identifying epidemiologic links.
D. Decolonization protocols: Not routinely recommended for Acinetobacter outbreaks.
CBIC Infection Control References:
CIC Study Guide, "Epidemiologic Investigations in Outbreaks," Chapter 4.
The infection preventionist observed a caregiver entering a room without performing hand hygiene. The BEST response would be to
Options:
post additional signage to remind caregivers to wash before entry.
provide immediate feedback and education to the caregiver.
install hand hygiene dispensers in more convenient areas.
design a unit-based education program.
Answer:
BExplanation:
Immediate feedback is a best practice in behavior correction and performance improvement. In hand hygiene non-compliance, real-time intervention allows for immediate correction, education, and reinforcement of infection prevention policies.
The APIC/JCR Workbook recommends:
“Provide simulation training… that provides immediate feedback—for example, how to properly insert a urinary catheter or perform hand hygiene.” This supports behavior change and staff learning.
The APIC Text emphasizes that real-time, direct feedback is more effective than passive measures like signage or delayed education campaigns.
The infection preventionist (IP) is invited to a planning meeting for a new oncology unit. The team is excited about the new design and wants lots of natural plants to be incorporated. What action should the IP take?
Options:
Allow the process to continue.
Ask about the air handling unit.
Ask whether artificial plants could be used instead.
Prohibit any discussion on the inclusion of natural plants.
Answer:
CExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) clearly emphasizes that oncology units house highly immunocompromised patients, making environmental sources of infection a critical concern during design and planning phases. Natural plants, soil, and standing water are well-recognized reservoirs for environmental fungi and gram-negative bacteria, including Aspergillus, Fusarium, and Pseudomonas species, all of which pose a serious infection risk to oncology patients.
Rather than allowing the process to continue unchecked (Option A) or completely shutting down discussion (Option D), the infection preventionist’s role is to guide the team toward safer alternatives while supporting collaborative planning. Asking whether artificial plants can be used instead (Option C) is the most appropriate action because it maintains the aesthetic goals of the design team while eliminating the infection risks associated with live plants.
Option B, asking about the air handling unit, is important in oncology design but does not directly address the specific and preventable risk posed by natural plants. The Study Guide notes that potted plants, dried flower arrangements, and soil-containing décor should be avoided in areas caring for severely immunocompromised patients.
For the CIC® exam, this question highlights the IP’s responsibility to anticipate environmental infection risks early in facility planning and recommend practical, evidence-based alternatives that protect patient safety without unnecessarily impeding design goals.
What factors contribute to the development of bacteria-containing biofilms within channels of endoscopes?
Options:
Frequent use of enzymatic detergents.
Inadequate cleaning and reprocessing protocols.
Use of chlorine- and monochloramine-based products.
Using a central reprocessing area rather than a local reprocessing area.
Answer:
BExplanation:
The Certification Study Guide (6th edition) identifies inadequate cleaning and reprocessing protocols as the primary factor contributing to the formation of bacteria-containing biofilms within endoscope channels. Endoscopes have long, narrow lumens and complex internal surfaces that are particularly vulnerable to biofilm formation when organic material is not thoroughly removed. Biofilms develop when microorganisms adhere to surfaces and become embedded within a protective extracellular matrix, which significantly reduces the effectiveness of disinfectants and sterilants.
The study guide emphasizes that cleaning is the most critical step in endoscope reprocessing. Failure to promptly and thoroughly clean channels—such as delayed cleaning, insufficient brushing, inadequate flushing, or improper detergent use—allows organic debris and moisture to remain, creating ideal conditions for microbial attachment and biofilm development. Once established, biofilms are difficult to eliminate and have been implicated in healthcare-associated infections linked to endoscopic procedures.
The incorrect options describe practices that do not promote biofilm formation. Enzymatic detergents, when used correctly, support removal of organic material. Chlorine-based products are not standard for endoscope channel reprocessing and are not the primary cause of biofilm development. Centralized reprocessing areas are considered best practice because they support standardized procedures, trained personnel, and quality control.
This concept is frequently tested on the CIC exam, reinforcing that breakdowns in basic cleaning and reprocessing practices pose the greatest risk for biofilm formation and patient harm.
Which of the following is NOT valuable when using a graph to display data?
Options:
Title with topic of data
Facility and time frame for data
Published trends for data comparison
X and Y axes labels and annotation where indicated
Answer:
CExplanation:
The Certification Study Guide (6th edition) explains that graphs are most effective when they clearly communicate who, what, when, and how regarding the data being presented. Essential elements include a descriptive title, identification of the facility and time frame, and properly labeled X and Y axes with annotations as needed. These components ensure that the viewer can accurately interpret the data without additional explanation.
Published trends for data comparison, while potentially useful in separate analyses or reports, are not required elements of an individual graph and do not inherently improve the clarity of data display. Including external published trends can actually confuse interpretation if definitions, populations, or surveillance methodologies differ from the local data being presented. The study guide cautions against mixing datasets with different assumptions or collection methods in a single visual display unless clearly contextualized.
Titles clarify the subject of the graph, facility and time frame provide essential context, and axis labels ensure the viewer understands what is being measured. These are foundational principles of data visualization emphasized in infection prevention reporting and communication.
CIC exam questions frequently test the ability to distinguish between essential graph components and supplementary analytical tools. Recognizing that published comparison trends are not required—and may be misleading—reinforces good data communication practices and supports accurate interpretation by leadership and frontline staff.
A director of the Infection Prevention and Control Department has received permission to hire more staff to a total of 3.8 full-time equivalents (FTEs), based on 40 hours/week. The director works 40 hours/week, one infection preventionist (IP) works 32 hours/week, another works 16 hours/week, and secretarial support works 40 hours/week. How many additional FTEs may the director hire?
Options:
0.4
0.6
0.8
1.0
Answer:
BExplanation:
The Certification Study Guide (6th edition) stresses that infection prevention leaders must understand basic workforce and FTE calculations to ensure appropriate staffing and compliance with approved resource allocations. An FTE is defined as 40 hours worked per week, and part-time hours must be converted proportionally.
First, calculate the FTEs already in use:
Director: 40 hours/week ÷ 40 = 1.0 FTE
Infection preventionist: 32 hours/week ÷ 40 = 0.8 FTE
Infection preventionist: 16 hours/week ÷ 40 = 0.4 FTE
Secretarial support: 40 hours/week ÷ 40 = 1.0 FTE
Total current FTEs:
1.0 + 0.8 + 0.4 + 1.0 = 3.2 FTEs
The approved staffing total is 3.8 FTEs. To determine how many additional FTEs may be hired, subtract current FTE usage from the approved total:
3.8 − 3.2 = 0.6 FTE
Therefore, the director may hire 0.6 additional FTE, which could be fulfilled by a part-time infection preventionist or split among staff roles, depending on organizational needs.
CIC exam questions frequently test practical management skills, including staffing calculations, budgeting awareness, and resource allocation. Accurate FTE calculations ensure compliance with administrative approvals and support safe, effective infection prevention program operations.
An outbreak of Candida auris is suspected in the infection preventionist's (IP) facility. The IP's investigation must be conducted in a standard method and communication is critical. Which first step is MOST important?
Options:
Conduct environmental cultures
Plan to prevent future outbreaks
Notify facility administration
Perform analytical studies
Answer:
CExplanation:
In an outbreak investigation, the first critical step is to notify facility administration and other key stakeholders. This ensures the rapid mobilization of resources, coordination with infection control teams, and compliance with regulatory reporting requirements.
Why the Other Options Are Incorrect?
A. Conduct environmental cultures – While environmental sampling may be necessary, it is not the first step. The outbreak must first be confirmed and administration alerted.
B. Plan to prevent future outbreaks – Prevention planning happens later after the outbreak has been investigated and controlled.
D. Perform analytical studies – Data analysis occurs after case definition and initial response measures are in place.
CBIC Infection Control Reference
APIC guidelines state that the first step in an outbreak investigation is confirming the outbreak and notifying key stakeholders.
What inflammatory reaction may occur in the eye after cataract surgery due to a breach in disinfection and sterilization of intraocular surgical instruments?
Options:
Endophthalmitis
Bacterial conjunctivitis
Toxic Anterior Segment Syndrome
Toxic Posterior Segment Syndrome
Answer:
CExplanation:
The correct answer is C, "Toxic Anterior Segment Syndrome," as this is the inflammatory reaction that may occur in the eye after cataract surgery due to a breach in disinfection and sterilization of intraocular surgical instruments. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, Toxic Anterior Segment Syndrome (TASS) is a sterile, acute inflammatory reaction that can result from contaminants introduced during intraocular surgery, such as endotoxins, residues from improper cleaning, or chemical agents left on surgical instruments due to inadequate disinfection or sterilization processes (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.3 - Ensure safe reprocessing of medical equipment). TASS typically presents within 12-48 hours post-surgery with symptoms like pain, redness, and anterior chamber inflammation, and it is distinct from infectious causes because it is not microbial in origin. A breach in reprocessing protocols, such as failure to remove detergents or improper sterilization, is a known risk factor, making it highly relevant to infection prevention efforts in surgical settings.
Option A (endophthalmitis) is an infectious inflammation of the internal eye structures, often caused by bacterial or fungal contamination, which can also result from poor sterilization but is distinguished from TASS by its infectious nature and longer onset (days to weeks). Option B (bacterial conjunctivitis) affects the conjunctiva and is typically a surface infection unrelated to intraocular surgery or sterilization breaches of surgical instruments. Option D (toxic posterior segment syndrome) is not a recognized clinical entity in the context of cataract surgery; inflammation in the posterior segment is more commonly associated with infectious endophthalmitis or other conditions, not specifically linked to reprocessing failures.
The focus on TASS aligns with CBIC’s emphasis on ensuring safe reprocessing to prevent adverse outcomes in surgical patients, highlighting the need for rigorous infection control measures (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). This is supported by CDC and American Academy of Ophthalmology guidelines, which identify TASS as a preventable complication linked to reprocessing errors (CDC Guidelines for Disinfection and Sterilization, 2019; AAO TASS Task Force Report, 2017).
An infection preventionist has decided to perform surveillance for central line–associated bloodstream infections (CLABSIs) in the facility’s ICU. Which of the following is the MOST appropriate denominator to calculate risk-adjusted rates?
Options:
Total number of ICU patients
Total number of patients with central lines
Number of patients with infections who have central lines
Number of days patients have central lines in place
Answer:
DExplanation:
The Certification Study Guide (6th edition) emphasizes that device-associated infection rates must be calculated using time-at-risk denominators to accurately reflect patient exposure. For CLABSI surveillance, the most appropriate denominator is central line days, defined as the total number of days patients have one or more central lines in place during the surveillance period.
Using central line days accounts for both the presence and duration of exposure, which is critical for risk adjustment. The longer a central line remains in place, the greater the opportunity for microbial entry and bloodstream infection. This denominator allows for valid trend analysis over time and meaningful benchmarking with national surveillance systems that use standardized definitions and denominators.
The other options are incorrect because they fail to measure exposure accurately. Total ICU patients and total patients with central lines do not account for how long the device was present. Counting only patients who developed infections incorrectly places outcomes in the denominator, which invalidates rate calculations.
The study guide reinforces that numerators represent infection events, while denominators represent populations or time at risk. For CLABSI, the standard rate is expressed as infections per 1,000 central line days, a core concept frequently tested on the CIC exam.
Accurate denominator selection ensures valid surveillance, supports quality improvement efforts, and enables comparison with national benchmarks—making central line days the correct and most appropriate choice.
Which of the following organisms is associated with a waterborne disease?
Options:
Bacillus anthracis
Cytomegalovirus
Nontuberculous mycobacteria
Stachybotrys
Answer:
CExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) identifies nontuberculous mycobacteria (NTM) as organisms commonly associated with waterborne exposure. NTM are environmental mycobacteria widely found in natural and treated water sources, including potable water systems, ice machines, showerheads, faucets, and medical equipment rinsed with tap water. Because these organisms are resistant to standard water disinfection methods and can form biofilms, they are particularly well adapted to survive in plumbing systems.
NTM have been implicated in healthcare-associated infections, especially among immunocompromised patients, and may cause pulmonary disease, skin and soft tissue infections, and invasive disease following exposure to contaminated water or medical devices. The Study Guide emphasizes the importance of water management programs and routine surveillance to prevent waterborne transmission of opportunistic pathogens such as NTM and Legionella.
The other answer options are incorrect. Bacillus anthracis is primarily associated with zoonotic and bioterrorism-related exposure, not waterborne transmission. Cytomegalovirus is transmitted through direct contact with bodily fluids rather than water. Stachybotrys is a mold associated with damp indoor environments but is not considered a waterborne pathogen in the context of infection transmission.
Understanding organisms linked to water systems is critical for infection preventionists, as waterborne pathogens present ongoing risks in healthcare facilities and are a key topic on the CIC® exam.
==========
An infection preventionist is developing training exercises for emergency preparedness and disaster response teams. The MOST effective instructional method for retaining information is:
Options:
Providing reading materials to the group.
Watching videos recorded by other hospitals.
Simulating an event to practice how to respond.
Administering a post-test after circulating the emergency response plan.
Answer:
CExplanation:
The Certification Study Guide (6th edition) emphasizes that active, experiential learning methods are the most effective for long-term retention of knowledge and skills, particularly in the context of emergency preparedness and disaster response. Simulation-based training allows participants to practice real-time decision-making, communication, and task execution in a controlled environment that closely mirrors actual emergency conditions.
Simulating an event—such as a mass casualty incident, infectious disease outbreak, or evacuation—engages learners cognitively, physically, and emotionally. The study guide notes that this type of hands-on training improves recall, reinforces correct behaviors, exposes system gaps, and builds team confidence. Simulation also supports interdisciplinary coordination and allows immediate feedback and debriefing, which further enhances learning retention.
The other instructional methods are less effective for retention. Reading materials and watching videos are passive learning approaches that may increase awareness but do not ensure competency during high-stress situations. Administering a post-test measures short-term knowledge acquisition but does not demonstrate the ability to apply that knowledge during an actual emergency.
CIC exam questions frequently highlight adult learning principles, stressing that people learn best by doing—especially when preparing for rare but high-risk events. Simulation-based exercises are therefore considered the gold standard for emergency preparedness training and are strongly recommended for disaster response teams.
An infection preventionist is observing the cleaning and disinfection process of semi-critical devices. To ensure these items have been reprocessed meeting the minimum requirements, which of the following is required?
Options:
Use of detergents with pH lower than 7
Initial cleaning must begin 24 hours after use
Initial cleaning must begin as soon as possible after use
Soaking in a solution of liquid chemical sterilant between 3 and 12 hours
Answer:
CExplanation:
The Certification Study Guide (6th edition) emphasizes that thorough cleaning is the most critical step in the reprocessing of all reusable medical devices, including semi-critical devices (those that contact mucous membranes or nonintact skin). A foundational requirement is that initial cleaning begins as soon as possible after use. Prompt cleaning prevents organic material—such as blood, secretions, and tissue—from drying on device surfaces and within lumens, which can shield microorganisms and significantly reduce the effectiveness of subsequent disinfection.
The study guide explains that delayed cleaning increases the risk of biofilm formation and makes removal of soil more difficult, potentially compromising patient safety. For this reason, point-of-use pre-cleaning and rapid transport to reprocessing are considered minimum expectations. Cleaning must occur before any high-level disinfection or sterilization; without effective cleaning, even correctly selected disinfectants may fail.
The other options are incorrect or misleading. There is no universal requirement for detergents with pH lower than 7; detergent selection should follow manufacturer instructions. Waiting 24 hours before cleaning is contrary to best practice and increases risk. Soaking devices in liquid chemical sterilants for extended periods does not address the prerequisite of cleaning and may not be appropriate for semi-critical devices unless specified by the manufacturer.
This question reflects a key CIC exam principle: timely cleaning is non-negotiable and is the cornerstone of safe device reprocessing.
Using tap water to rinse suction tubing can cause transmission of
Options:
Klebsiella spp.
Staphylococcus spp.
Pseudomonas spp.
Streptococcus spp.
Answer:
CExplanation:
Pseudomonas spp., particularly Pseudomonas aeruginosa, is a common waterborne pathogen. Using tap water to rinse suction tubing has been associated with outbreaks of Pseudomonas infections.
From the APIC Text:
“Water bottles improperly filled with tap water and used for rinsing tracheal suction tubing resulted in an outbreak of P. cepacia... Tubing permanently attached to showers... implicated in a serious outbreak of P. aeruginosa bloodstream infection.”
An infection preventionist (IP) receives a phone call from a local health department alerting the hospital of the occurrence of a sewer main break. Contamination of the city water supply is a possibility. Which of the following actions should the IP perform FIRST?
Options:
Notify the Emergency and Admissions departments to report diarrhea cases to infection control.
Review microbiology laboratory reports for enteric organisms in the past week.
Contact the Employee Health department and ask for collaboration in case-finding.
Review the emergency preparedness plan with engineering for sources of potable water.
Answer:
BExplanation:
The correct answer is B, "Review microbiology laboratory reports for enteric organisms in the past week," as this is the first action the infection preventionist (IP) should perform following the alert of a sewer main break and potential contamination of the city water supply. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, a rapid assessment of existing data is a critical initial step in investigating a potential waterborne outbreak. Reviewing microbiology laboratory reports for enteric organisms (e.g., Escherichia coli, Salmonella, or Shigella) helps the IP identify any recent spikes in infections that could indicate water supply contamination, providing an evidence-based starting point for the investigation (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.2 - Analyze surveillance data). This step leverages available hospital data to assess the scope and urgency of the situation before initiating broader actions.
Option A (notify the Emergency and Admissions departments to report diarrhea cases to infection control) is an important subsequent step to enhance surveillance, but it relies on proactive reporting and does not provide immediate evidence of an ongoing issue. Option C (contact the Employee Health department and ask for collaboration in case-finding) is valuable for involving additional resources, but it should follow the initial data review to prioritize case-finding efforts based on identified trends. Option D (review the emergency preparedness plan with engineering for sources of potable water) is a critical preparedness action, but it is more relevant once contamination is confirmed or as a preventive measure, not as the first step in assessing the current situation.
The focus on reviewing laboratory reports aligns with CBIC’s emphasis on using surveillance data to guide infection prevention responses, enabling the IP to quickly determine if the sewer main break has already impacted patient health and to escalate actions accordingly (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.1 - Conduct surveillance for healthcare-associated infections and epidemiologically significant organisms). This approach is consistent with CDC guidelines for responding to waterborne outbreak alerts (CDC Environmental Public Health Guidelines, 2020).
When conducting a literature search which of the following study designs may provide the best evidence of a direct causal relationship between the experimental factor and the outcome?
Options:
A case report
A descriptive study
A case control study
A randomized-controlled trial
Answer:
DExplanation:
To determine the best study design for providing evidence of a direct causal relationship between an experimental factor and an outcome, it is essential to understand the strengths and limitations of each study design listed. The goal is to identify a design that minimizes bias, controls for confounding variables, and establishes a clear cause-and-effect relationship.
A. A case report: A case report is a detailed description of a single patient or a small group of patients with a particular condition or outcome, often including the experimental factor of interest. While case reports can generate hypotheses and highlight rare occurrences, they lack a control group and are highly susceptible to bias. They do not provide evidence of causality because they are observational and anecdotal in nature. This makes them the weakest design for establishing a direct causal relationship.
B. A descriptive study: Descriptive studies, such as cross-sectional or cohort studies, describe the characteristics or outcomes of a population without manipulating variables. These studies can identify associations between an experimental factor and an outcome, but they do not establish causality due to the absence of randomization or control over confounding variables. For example, a descriptive study might show that a certain infection rate is higher in a group exposed to a specific factor, but it cannot prove the factor caused the infection without further evidence.
C. A case control study: A case control study compares individuals with a specific outcome (cases) to those without (controls) to identify factors that may contribute to the outcome. This retrospective design is useful for studying rare diseases or outcomes and can suggest associations. However, it is prone to recall bias and confounding, and it cannot definitively prove causation because the exposure is not controlled or randomized. It is stronger than case reports or descriptive studies but still falls short of establishing direct causality.
D. A randomized-controlled trial (RCT): An RCT is considered the gold standard for establishing causality in medical and scientific research. In an RCT, participants are randomly assigned to either an experimental group (exposed to the factor) or a control group (not exposed or given a placebo). Randomization minimizes selection bias and confounding variables, while the controlled environment allows researchers to isolate the effect of the experimental factor on the outcome. The ability to compare outcomes between groups under controlled conditions provides the strongest evidence of a direct causal relationship. This aligns with the principles of evidence-based practice, which the CBIC (Certification Board of Infection Control and Epidemiology) emphasizes for infection prevention and control strategies.
Based on this analysis, the randomized-controlled trial (D) is the study design that provides the best evidence of a direct causal relationship. This conclusion is consistent with the CBIC's focus on high-quality evidence to inform infection control practices, as RCTs are prioritized in the hierarchy of evidence for establishing cause-and-effect relationships.
CBIC Infection Prevention and Control (IPC) Core Competency Model (updated guidelines, 2023), which emphasizes the use of high-quality evidence, including RCTs, for validating infection control interventions.
CBIC Examination Content Outline, Domain I: Identification of Infectious Disease Processes, which underscores the importance of evidence-based study designs in infection control research.
An infection preventionist, Cancer Committee, and Intravenous Therapy Department are studying the incidence of infections in patients with triple lumen catheters. Which of the following is essential to the quality improvement process?
Options:
Establish subjective criteria for outcome measurement.
Recommendations for intervention must be approved by the governing board.
Study criteria must be approved monthly by the Cancer Committee.
A monitoring system must be in place following implementation of interventions.
Answer:
DExplanation:
The correct answer is D, "A monitoring system must be in place following implementation of interventions," as this is essential to the quality improvement (QI) process. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, a key component of any QI initiative, such as studying the incidence of infections in patients with triple lumen catheters, is the continuous evaluation of interventions to assess their effectiveness and ensure sustained improvement. A monitoring system allows the infection preventionist (IP), Cancer Committee, and Intravenous Therapy Department to track infection rates, identify trends, and make data-driven adjustments to infection control practices post-intervention (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.4 - Evaluate the effectiveness of infection prevention and control interventions). This step is critical to validate the success of implemented strategies, such as catheter care protocols, and to prevent healthcare-associated infections (HAIs).
Option A (establish subjective criteria for outcome measurement) is not ideal because QI processes rely on objective, measurable outcomes (e.g., infection rates per 1,000 catheter days) rather than subjective criteria to ensure reliability and reproducibility. Option B (recommendations for intervention must be approved by the governing board) is an important step for institutional support and resource allocation, but it is a preparatory action rather than an essential component of the ongoing QI process itself. Option C (study criteria must be approved monthly by the Cancer Committee) suggests an unnecessary administrative burden; while initial approval of study criteria is important, monthly re-approval is not a standard QI requirement unless mandated by specific policies, and it does not directly contribute to the improvement process.
The emphasis on a monitoring system aligns with CBIC’s focus on using surveillance data to guide and refine infection prevention efforts, ensuring that interventions for triple lumen catheter-related infections are effective and adaptable (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.5 - Use data to guide infection prevention and control strategies). This approach supports a cycle of continuous improvement, which is foundational to reducing catheter-associated bloodstream infections (CABSI) in healthcare settings.
Based on the Spaulding classification, which of the following pairings is an example of a semi-critical item and its minimal level of disinfection?
Options:
Bedside table; high-level disinfection
Surgical instrument; sterilization
Endocavity probe; high-level disinfection
Bedpan; intermediate-level disinfection
Answer:
CExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes the importance of applying Spaulding’s classification to determine the appropriate minimum level of processing for medical devices. Under this system, devices are categorized as critical, semi-critical, or noncritical based on the degree of infection risk associated with their use.
Semi-critical items are those that come into contact with mucous membranes or non-intact skin but do not ordinarily penetrate sterile tissue. Examples include endocavity probes, such as transvaginal or transrectal ultrasound probes. Because mucous membranes are more susceptible to infection than intact skin, semi-critical items require at least high-level disinfection after thorough cleaning to eliminate all microorganisms except large numbers of bacterial spores.
Option C correctly pairs an endocavity probe with high-level disinfection, which is the minimum acceptable level of processing for this classification. Option A is incorrect because a bedside table is a noncritical item and requires only low-level disinfection. Option B describes a critical item, which correctly requires sterilization but does not meet the question’s focus on semi-critical devices. Option D is incorrect because bedpans are noncritical items, and intermediate-level disinfection exceeds the minimum requirement.
Understanding Spaulding’s classification and matching devices to the correct level of disinfection is a high-yield topic on the CIC® exam and essential for safe infection prevention practice.
==========
A family, including an infant of 8 months, is going on a vacation to Europe. An infection preventionist would recommend:
Options:
Exposure to rabies should be avoided.
Family members should be vaccinated for yellow fever.
The infant should not travel until at least 12 months of age.
Family immunization records should be reviewed by their provider.
Answer:
DExplanation:
When advising a family, including an 8-month-old infant, planning a vacation to Europe, an infection preventionist (IP) must consider travel-related health risks and vaccination recommendations tailored to the destination and age-specific guidelines. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes the "Education and Training" domain, which includes providing evidence-based advice to prevent infections, aligning with the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) travel health recommendations.
Option D, "Family immunization records should be reviewed by their provider," is the most appropriate recommendation. Europe, as a region, includes countries with varying health risks, but it is generally considered a low-risk area for many vaccine-preventable diseases compared to tropical regions. The CDC’s "Travelers’ Health" guidelines (2023) recommend that all travelers, including infants, have their immunization status reviewed by a healthcare provider prior to travel to ensure compliance with routine vaccinations (e.g., measles, mumps, rubella [MMR], diphtheria, tetanus, pertussis [DTaP], and polio) and to assess any destination-specific needs. For an 8-month-old, the review would confirm that the infant has received age-appropriate vaccines (e.g., the first doses of DTaP, Hib, PCV, and IPV, typically starting at 2 months) and is on schedule for the 6- and 12-month doses. This step ensures the family’s overall protection and identifies any gaps, making it a proactive and universally applicable recommendation.
Option A, "Exposure to rabies should be avoided," is a general travel safety tip applicable to any destination where rabies is endemic (e.g., parts of Eastern Europe or rural areas with wildlife). However, rabies risk in most European countries is low, and pre-exposure vaccination is not routinely recommended for travelers unless specific high-risk activities (e.g., handling bats) are planned. The CDC advises avoiding animal bites rather than vaccinating unless indicated, making this less specific and urgent than a records review. Option B, "Family members should be vaccinated for yellow fever," is incorrect. Yellow fever is not endemic in Europe, and vaccination is not required or recommended for travel to any European country. The WHO International Health Regulations (2005) and CDC list yellow fever vaccination as mandatory only for travelers from or to certain African and South American regions, rendering this irrelevant. Option C, "The infant should not travel until at least 12 months of age," lacks a clear evidence base. While some vaccines (e.g., MMR) are typically given at 12 months, the 8-month-old can travel safely if up-to-date on age-appropriate immunizations. The CDC allows travel for infants as young as 6 weeks with medical clearance, and delaying travel to 12 months is not a standard recommendation unless specific risks (e.g., disease outbreaks) are present, which are not indicated here.
The CBIC Practice Analysis (2022) and CDC Travelers’ Health resources prioritize pre-travel health assessments, including immunization reviews, as the foundation for safe travel. Option D ensures a comprehensive approach tailored to the family’s needs, making it the best recommendation for a trip to Europe.
Which of the following correctly characterizes endovaginal ultrasound probes?
Options:
They must be sterilized with a liquid chemical sterilant after use.
They are protected from viral contamination if covered by a sheath.
They are critical items based on the Spaulding Classification System.
They may be contaminated with human papillomavirus pre-examination.
Answer:
DExplanation:
The Certification Study Guide (6th edition) classifies endovaginal ultrasound probes as semi-critical devices because they come into contact with mucous membranes. As such, they require high-level disinfection (HLD) between patients, not sterilization, unless the manufacturer specifically requires it. This immediately eliminates option A, which incorrectly states sterilization is required.
Option B is incorrect because probe covers or sheaths do not eliminate the risk of contamination. Numerous studies referenced in infection prevention literature and reflected in the study guide demonstrate that probe covers can fail, tear, or leak, allowing microorganisms—including viruses—to contaminate the probe surface. Therefore, HLD is required regardless of sheath use.
Option C is incorrect because critical items, by definition, enter sterile tissue or the vascular system. Endovaginal probes contact mucous membranes only and are therefore not critical items under the Spaulding Classification System.
Option D is correct because endovaginal probes may be contaminated with human papillomavirus (HPV) prior to examination, even when probe covers are used. HPV is particularly concerning due to its resistance to some low-level disinfectants and its ability to persist on surfaces. The study guide highlights HPV as a key organism driving strict reprocessing requirements for these probes.
This question reflects a high-yield CIC exam concept: probe covers do not replace high-level disinfection, and viral contamination—including HPV—remains a significant risk.
Given the formula for calculating incidence rates, the Y represents which of the following?

Options:
Population served
Number of infected patients
Population at risk
Number of events
Answer:
CExplanation:
Incidence rate is a fundamental epidemiological measure used to quantify the frequency of new cases of a disease within a specified population over a defined time period. The Certification Board of Infection Control and Epidemiology (CBIC) supports the use of such metrics in the "Surveillance and Epidemiologic Investigation" domain, aligning with the Centers for Disease Control and Prevention (CDC) "Principles of Epidemiology in Public Health Practice" (3rd Edition, 2012). The formula provided, XY×K=Rate\frac{X}{Y} \times K = RateYX×K=Rate, represents the standard incidence rate calculation, where KKK is a constant (e.g., 1,000 or 100,000) to express the rate per unit population, and the question asks what YYY represents among the given options.
In the incidence rate formula, XXX typically represents the number of new cases (or events) of the disease occurring during a specific period, and YYY represents the population at risk during that same period. The ratio XY\frac{X}{Y}YX yields the rate per unit of population, which is then multiplied by KKK to standardize the rate (e.g., cases per 1,000 persons). The CDC defines the denominator (YYY) as the population at risk, which includes individuals susceptible to the disease over the observation period. Option B ("Number of infected patients") might suggest XXX if it specified new cases, but as the denominator YYY, it is incorrect because incidence focuses on new cases relative to the at-risk population, not the total number of infected individuals (which could include prevalent cases). Option C ("Population at risk") correctly aligns with YYY, representing the base population over which the rate is calculated.
Option A, "Population served," is a broader term that might include the total population under care (e.g., in a healthcare facility), but it is not specific to those at risk for new infections, making it less precise. Option D, "Number of events," could align with XXX (new cases or events), but as the denominator YYY, it does not fit the formula’s structure. The CBIC Practice Analysis (2022) and CDC guidelines reinforce that the denominator in incidence rates is the population at risk, ensuring accurate measurement of new disease occurrence.
Which performance improvement model should the infection preventionist use to aid in the evaluation of the infection control plan?
Options:
Six Sigma
Failure mode and effects analysis
Plan, Do, Study, Act
Root Cause Analysis
Answer:
CExplanation:
The Plan, Do, Study, Act (PDSA) model is a widely used performance improvement tool in infection prevention. It focuses on continuous quality improvement through planning, implementing, analyzing data, and making adjustments. This model aligns with infection control program evaluations and The Joint Commission’s infection prevention and control standards.
Why the Other Options Are Incorrect?
A. Six Sigma – A data-driven process improvement method but not as commonly used in infection control as PDSA.
B. Failure Mode and Effects Analysis (FMEA) – Used to identify risks before implementation, rather than ongoing evaluation.
D. Root Cause Analysis (RCA) – Used to analyze failures after they occur, rather than guiding continuous improvement.
CBIC Infection Control Reference
The PDSA cycle is a recognized model for evaluating and improving infection control plans.
Following an outbreak of Hepatitis A, the water supply is sampled. A high count of which of the following isolates would indicate that the water was a potential source?
Options:
Coliforms
Pseudomonads
Legionella
Acinetobacter
Answer:
AExplanation:
Coliform bacteria are indicators of fecal contamination in water, making them a critical measure of water safety. Hepatitis A is a virus primarily transmitted via the fecal-oral route, often through contaminated food or water.
Step-by-Step Justification:
Fecal Contamination and Hepatitis A:
Hepatitis A virus (HAV) spreads through ingestion of water contaminated with fecal matter. High coliform counts indicate fecal contamination and increase the risk of HAV outbreaks.
Use of Coliforms as Indicators:
Public health agencies use total coliforms and Escherichia coli (E. coli) as primary indicators of water safety because they signal fecal pollution.
Waterborne Transmission of Hepatitis A:
Hepatitis A outbreaks have been traced to contaminated drinking water, ice, and improperly treated wastewater. Coliform detection signals a need for immediate action.
Why Other Options Are Incorrect:
B. Pseudomonads:
Pseudomonads (e.g., Pseudomonas aeruginosa) are environmental bacteria but are not indicators of fecal contamination.
C. Legionella:
Legionella species cause Legionnaires' disease through inhalation of contaminated aerosols, not through fecal-oral transmission.
D. Acinetobacter:
Acinetobacter species are opportunistic pathogens in healthcare settings but are not indicators of waterborne fecal contamination.
CBIC Infection Control References:
APIC Text, "Water Systems and Infection Control Measures".
APIC Text, "Hepatitis A Transmission and Waterborne Outbreaks".
An infection preventionist should collaborate with a public health agency in primary prevention efforts by:
Options:
Conducting outbreak investigations.
Performing surveillance for tuberculosis through tuberculin skin test.
Promoting vaccination of health care workers and patients.
Offering blood and body fluid post-exposure prophylaxis.
Answer:
CExplanation:
Primary prevention focuses on preventing the initial occurrence of disease or injury before it manifests, distinguishing it from secondary (early detection) and tertiary (mitigation of complications) prevention. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes the "Prevention and Control of Infectious Diseases" domain, which includes collaboration with public health agencies to implement preventive strategies, aligning with the Centers for Disease Control and Prevention (CDC) framework for infection prevention. The question requires identifying the activity that best fits primary prevention efforts.
Option C, "Promoting vaccination of health care workers and patients," is the correct answer. Vaccination is a cornerstone of primary prevention, as it prevents the onset of vaccine-preventable diseases (e.g., influenza, hepatitis B, measles) by inducing immunity before exposure. The CDC’s "Immunization of Health-Care Personnel" (2011) and "General Recommendations on Immunization" (2021) highlight the role of vaccination in protecting both healthcare workers and patients, reducing community transmission and healthcare-associated infections. Collaboration with public health agencies, which often oversee vaccination campaigns and supply distribution, enhances this effort, making it a proactive primary prevention strategy.
Option A, "Conducting outbreak investigations," is a secondary prevention activity. Outbreak investigations occur after cases are identified to control spread and mitigate impact, focusing on containment rather than preventing initial disease occurrence. The CDC’s "Principles of Epidemiology in Public Health Practice" (3rd Edition, 2012) classifies this as a response to an existing problem. Option B, "Performing surveillance for tuberculosis through tuberculin skin test," is also secondary prevention. Surveillance, including tuberculin skin testing, aims to detect latent or active tuberculosis early to prevent progression or transmission, not to prevent initial infection. The CDC’s "Guidelines for Preventing the Transmission of Mycobacterium tuberculosis" (2005) supports this as a screening tool. Option D, "Offering blood and body fluid post-exposure prophylaxis," is tertiary prevention. Post-exposure prophylaxis (e.g., for HIV or hepatitis B) is administered after potential exposure to prevent disease development, focusing on mitigating consequences rather than preventing initial exposure, as outlined in the CDC’s "Updated U.S. Public Health Service Guidelines" (2013).
The CBIC Practice Analysis (2022) and CDC guidelines prioritize vaccination as a primary prevention strategy, and collaboration with public health agencies amplifies its reach. Option C best reflects this preventive focus, making it the correct choice.
Peripherally inserted central catheter (PICC)-associated bloodstream infections (BSIs) have been increasing over the past four months. Which of the following interventions is MOST likely to have contributed to the increase?
Options:
Use of chlorhexidine skin antisepsis during insertion of the PICC
Daily bathing adult intensive care unit patients with chlorhexidine
Replacement of the intravenous administration sets every 72 hours
Use of a positive pressure device on the PICC
Answer:
CExplanation:
Peripherally inserted central catheter (PICC)-associated bloodstream infections (BSIs) are a significant concern in healthcare settings, and identifying factors contributing to their increase is critical for infection prevention. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes the "Surveillance and Epidemiologic Investigation" and "Prevention and Control of Infectious Diseases" domains, which align with the Centers for Disease Control and Prevention (CDC) guidelines for preventing intravascular catheter-related infections. The question asks for the intervention most likely to have contributed to the rise in PICC-associated BSIs over four months, requiring an evaluation of each option based on evidence-based practices.
Option C, "Replacement of the intravenous administration sets every 72 hours," is the most likely contributor to the increase. The CDC’s "Guidelines for the Prevention of Intravascular Catheter-Related Infections" (2017) recommend that intravenous administration sets (e.g., tubing for fluids or medications) be replaced no more frequently than every 72-96 hours unless clinically indicated (e.g., contamination or specific therapy requirements). Frequent replacement, such as every 72 hours as a routine practice, can introduce opportunities for contamination during the change process, especially if aseptic technique is not strictly followed. Studies cited in the CDC guidelines, including those by O’Grady et al. (2011), indicate that unnecessary manipulation of catheter systems increases the risk of introducing pathogens, potentially leading to BSIs. A change to a 72-hour replacement schedule, if not previously standard, could explain the observed increase over the past four months.
Option A, "Use of chlorhexidine skin antisepsis during insertion of the PICC," is a recommended practice to reduce BSIs. Chlorhexidine, particularly in a 2% chlorhexidine gluconate with 70% alcohol solution, is the preferred skin antiseptic for catheter insertion due to its broad-spectrum activity and residual effect, as supported by the CDC (2017). This intervention should decrease, not increase, infection rates, making it an unlikely contributor. Option B, "Daily bathing adult intensive care unit patients with chlorhexidine," is another evidence-based strategy to reduce healthcare-associated infections, including BSIs, by decolonizing the skin of pathogens like Staphylococcus aureus. The CDC and SHEA (Society for Healthcare Epidemiology of America) guidelines (2014) endorse chlorhexidine bathing in intensive care units, suggesting it should lower, not raise, BSI rates. Option D, "Use of a positive pressure device on the PICC," aims to prevent catheter occlusion and reduce the need for frequent flushing, which could theoretically decrease infection risk by minimizing manipulation. However, there is no strong evidence linking positive pressure devices to increased BSIs; if improperly used or maintained, they might contribute marginally, but this is less likely than the impact of frequent tubing changes.
The CBIC Practice Analysis (2022) and CDC guidelines highlight that deviations from optimal catheter maintenance practices, such as overly frequent administration set replacements, can increase infection risk. Given the four-month timeframe and the focus on an intervention’s potential negative impact, Option C stands out as the most plausible contributor due to the increased manipulation and contamination risk associated with routine 72-hour replacements.
An infection control manager is training a new infection preventionist. In discussing surveillance strategies, which of the following types of hospital infection surveillance usually provides maximum benefit with minimum resources?
Options:
High-risk patient focus
Antibiotic monitoring
Prevalence surveys
Nursing care plan review
Answer:
AExplanation:
A high-risk patient focus maximizes benefits while minimizing resource use in infection surveillance.
Step-by-Step Justification:
Efficiency of High-Risk Surveillance:
Targeting ICU, immunocompromised patients, or surgical units helps detect infections where the risk is highest, leading to earlier interventions.
Resource Allocation:
Full hospital-wide surveillance is resource-intensive; focusing on high-risk groups is more efficient.
Why Other Options Are Incorrect:
B. Antibiotic monitoring:
Important for stewardship, but not the primary focus of infection surveillance.
C. Prevalence surveys:
Snapshot data only; does not provide ongoing monitoring.
D. Nursing care plan review:
Less direct in identifying infection trends.
CBIC Infection Control References:
APIC Text, "Surveillance Strategies for Infection Prevention".
What is a characteristic of immediate-use steam sterilization?
Options:
Alternative to purchasing expensive instrument sets.
Can be used for the following surgery if properly stored.
Substitute for maintaining sufficient amounts of sterile instruments.
Performed in emergencies where cleaning is the most critical step.
Answer:
CExplanation:
The correct answer is C, "Substitute for maintaining sufficient amounts of sterile instruments," as this is a characteristic of immediate-use steam sterilization (IUSS). According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, IUSS, formerly known as flash sterilization, is a process designed to rapidly sterilize items that are needed urgently when pre-sterilized inventory is unavailable or insufficient. It serves as a temporary solution to address gaps in sterile instrument availability, such as during unexpected surges in surgical demand or equipment shortages, provided strict protocols are followed (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.3 - Ensure safe reprocessing of medical equipment). However, IUSS is not a routine practice and should be minimized due to its limitations, including the lack of immediate biologic indicator results.
Option A (alternative to purchasing expensive instrument sets) is incorrect because IUSS is not intended as a cost-saving measure or a replacement for acquiring necessary equipment; it is a contingency process. Option B (can be used for the following surgery if properly stored) is misleading, as IUSS items are intended for immediate use and not for storage or use in subsequent procedures, which requires standard sterilization cycles with proper packaging and validation. Option D (performed in emergencies where cleaning is the most critical step) overemphasizes cleaning and mischaracterizes IUSS; while cleaning is a critical initial step, the process is defined by its rapid sterilization for emergency use, not solely by cleaning priority.
The characteristic of substituting for insufficient sterile instruments aligns with CBIC’s focus on ensuring safe reprocessing practices while acknowledging the practical challenges in healthcare settings (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). This is supported by AAMI ST79, which outlines IUSS as a last-resort measure to maintain surgical readiness (AAMI ST79:2017).
A patient who is pregnant has multidrug-resistant tuberculosis. She presents to the hospital for delivery. She continues to have a productive cough and has sputum smears positive for acid-fast bacilli (AFB), despite treatment. An infection preventionist should recommend which of the following?
Options:
Immediately separate the infant from the mother at delivery and place the infant in Airborne Precautions until discharge.
The infant should “room in” with the mother and the mother should wear a mask at all times.
The infant may go from Airborne Precautions in the nursery to the mother’s room, as long as the mother wears a mask when the infant is in the room.
No isolation is required for the infant; however, the mother should be placed in Airborne Precautions.
Answer:
CExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) addresses management of tuberculosis (TB) in the peripartum setting, emphasizing protection of the neonate while supporting maternal–infant bonding when safely possible. In this scenario, the mother has active, infectious multidrug-resistant TB, as evidenced by persistent productive cough and positive AFB smears, and therefore requires Airborne Precautions.
Newborns are at high risk for TB infection due to immature immune systems; however, complete and prolonged separation is not always required. The recommended approach is to initially place the infant in Airborne Precautions in the nursery and allow limited, controlled contact with the mother once appropriate safeguards are in place. When the infant is brought to the mother’s room, the mother must wear a surgical mask to reduce droplet nuclei exposure, and exposure time should be minimized.
Option A is overly restrictive and not required unless safe controls cannot be maintained. Option B is incorrect because unrestricted rooming-in places the infant at unacceptable risk. Option D is incorrect because the infant does require protection when the mother is infectious.
For the CIC® exam, it is critical to recognize that TB management balances infection prevention with family-centered care. Controlled infant exposure with maternal masking is the recommended practice when mothers remain infectious at delivery.
Which of the following products or methods is effective for sterilization of heat-sensitive critical items?
Options:
Phenolics
Chlorine-based
Quaternary ammonium
Hydrogen peroxide gas plasma
Answer:
DExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) explains that critical items—those that enter sterile tissue or the vascular system—must be sterile at the time of use. When these items are heat-sensitive and cannot tolerate steam sterilization, low-temperature sterilization technologies are required. Among the options listed, hydrogen peroxide gas plasma is an FDA-cleared, low-temperature sterilization method specifically designed for heat- and moisture-sensitive medical devices.
Hydrogen peroxide gas plasma sterilization achieves sterilization by generating reactive free radicals that destroy microorganisms, including bacteria, viruses, fungi, and spores. The study guide emphasizes that this method provides true sterilization rather than disinfection and is widely used for delicate instruments such as certain endoscopes, optical devices, and electronic equipment. It also offers advantages such as short cycle times and minimal toxic residues.
The other options are incorrect because they do not achieve sterilization. Phenolics, chlorine-based products, and quaternary ammonium compounds are disinfectants, not sterilants, and are inappropriate for critical items. Even at high concentrations, these agents cannot reliably destroy bacterial spores and therefore do not meet the definition of sterilization.
This question highlights a key CIC exam concept: critical items require sterilization, and when heat cannot be used, approved low-temperature sterilization technologies such as hydrogen peroxide gas plasma are required to ensure patient safety.
An adult with an incomplete vaccination history presents with an uncontrollable, rapid and violent cough, fever, and runny nose. Healthcare personnel should suspect
Options:
Pertussis.
Rhinovirus.
Bronchitis.
Adenovirus.
Answer:
AExplanation:
The correct answer is A, "Pertussis," as healthcare personnel should suspect this condition based on the presented symptoms and the patient’s incomplete vaccination history. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, pertussis, caused by the bacterium Bordetella pertussis, is characterized by an initial phase of mild respiratory symptoms (e.g., runny nose, low-grade fever) followed by a distinctive uncontrollable, rapid, and violent cough, often described as a "whooping" cough. This presentation is particularly concerning in adults with incomplete vaccination histories, as the pertussis vaccine’s immunity (e.g., DTaP or Tdap) wanes over time, increasing susceptibility (CBIC Practice Analysis, 2022, Domain I: Identification of Infectious Disease Processes, Competency 1.1 - Identify infectious disease processes). Pertussis is highly contagious and poses a significant risk in healthcare settings, necessitating prompt suspicion and isolation to prevent transmission.
Option B (rhinovirus) typically causes the common cold with symptoms like runny nose, sore throat, and mild cough, but it lacks the violent, paroxysmal cough characteristic of pertussis. Option C (bronchitis) may involve cough and fever, often due to viral or bacterial infection, but it is not typically associated with the rapid and violent cough pattern or linked to vaccination status in the same way as pertussis. Option D (adenovirus) can cause respiratory symptoms, including cough and fever, but it is more commonly associated with conjunctivitis or pharyngitis and does not feature the hallmark violent cough of pertussis.
The suspicion of pertussis aligns with CBIC’s emphasis on recognizing infectious disease patterns to initiate timely infection control measures, such as droplet precautions and prophylaxis for exposed individuals (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). Early identification is critical, especially in healthcare settings, to protect vulnerable patients and staff, and the incomplete vaccination history supports this differential diagnosis given pertussis’s vaccine-preventable nature (CDC Pink Book: Pertussis, 2021).
Which of the following infectious diseases is associated with environmental fungi?
Options:
Listeriosis
Hantavirus
Mucormycosis
Campylobacter
Answer:
CExplanation:
The correct answer is C, "Mucormycosis," as it is the infectious disease associated with environmental fungi. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, mucormycosis is caused by fungi belonging to the order Mucorales, which are commonly found in the environment, including soil, decaying organic matter, and contaminated water. These fungi can become opportunistic pathogens, particularly in immunocompromised individuals, leading to severe infections such as rhinocerebral, pulmonary, or cutaneous mucormycosis (CBIC Practice Analysis, 2022, Domain I: Identification of Infectious Disease Processes, Competency 1.1 - Identify infectious disease processes). Environmental exposure, such as inhalation of fungal spores or contact with contaminated materials, is a primary mode of transmission, making it directly linked to environmental fungi.
Option A (Listeriosis) is caused by the bacterium Listeria monocytogenes, typically associated with contaminated food products (e.g., unpasteurized dairy or deli meats) rather than environmental fungi. Option B (Hantavirus) is a viral infection transmitted through contact with rodent excreta, not fungi, and is linked to environmental reservoirs like rodent-infested areas. Option D (Campylobacter) is a bacterial infection caused by Campylobacter species, often associated with undercooked poultry or contaminated water, and is not related to fungi.
The association of mucormycosis with environmental fungi underscores the importance of infection prevention strategies, such as controlling environmental contamination and protecting vulnerable patients, which aligns with CBIC’s focus on identifying and mitigating risks from infectious agents in healthcare settings (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). This knowledge is critical for infection preventionists to guide environmental cleaning and patient care protocols.
After defining and identifying cases in a possible cluster of infections, an infection preventionist should NEXT establish:
Options:
The route of transmission.
An appropriate control group.
A hypothesis that will explain the majority of cases.
Whether observed incidence exceeds expected incidence.
Answer:
CExplanation:
When investigating a possible cluster of infections, an infection preventionist (IP) follows a structured epidemiological approach to identify the cause and implement control measures. The Certification Board of Infection Control and Epidemiology (CBIC) outlines this process within the "Surveillance and Epidemiologic Investigation" domain, which aligns with the Centers for Disease Control and Prevention (CDC) guidelines for outbreak investigation. The steps typically include defining and identifying cases, formulating a hypothesis, testing the hypothesis, and implementing control measures. The question specifies the next step after defining and identifying cases, requiring an evaluation of the logical sequence.
Option C, "A hypothesis that will explain the majority of cases," is the next critical step. After confirming a cluster through case definition and identification (e.g., by time, place, and person), the IP should develop a working hypothesis to explain the observed pattern. This hypothesis might propose a common source (e.g., contaminated equipment), a mode of transmission (e.g., airborne), or a specific population at risk. The CDC’s "Principles of Epidemiology in Public Health Practice" (3rd Edition, 2012) emphasizes that formulating a hypothesis is essential to guide further investigation, such as identifying risk factors or environmental sources. This step allows the IP to focus resources on testing the most plausible explanation before proceeding to detailed analysis or interventions.
Option A, "The route of transmission," is an important element of the investigation but typically follows hypothesis formulation. Determining the route (e.g., contact, droplet, or common vehicle) requires data collection and analysis to test the hypothesis, making it a subsequent step rather than the immediate next action. Option B, "An appropriate control group," is relevant for analytical studies (e.g., case-control studies) to compare exposed versus unexposed individuals, but this is part of hypothesis testing, which occurs after the hypothesis is established. Selecting a control group prematurely, without a hypothesis, lacks direction and efficiency. Option D, "Whether observed incidence exceeds expected incidence," is a preliminary step to define a cluster, often done during case identification using baseline data or statistical thresholds (e.g., exceeding the mean plus two standard deviations). Since the question assumes cases are already defined and identified, this step is complete, and the focus shifts to hypothesis development.
The CBIC Practice Analysis (2022) and CDC guidelines prioritize hypothesis formulation as the logical next step after case identification, enabling a targeted investigation. This approach ensures that the IP can efficiently address the cluster’s cause, making Option C the correct answer.
Which of the following individuals should be excluded from receiving live attenuated influenza virus?
Options:
Pregnant persons
Healthy persons aged 2 to 49
Persons with allergies to chicken feathers
Persons simultaneously receiving an inactivated vaccine
Answer:
AExplanation:
The correct answer is A, "Pregnant persons," as they should be excluded from receiving the live attenuated influenza virus (LAIV) vaccine. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, which align with recommendations from the Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP), the LAIV, commonly known as the nasal spray flu vaccine, contains a live attenuated form of the influenza virus. This vaccine is contraindicated in pregnant individuals due to the theoretical risk of the attenuated virus replicating and potentially harming the fetus, despite limited evidence of adverse outcomes (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). Pregnant persons are instead recommended to receive the inactivated influenza vaccine (IIV), which is considered safe during pregnancy.
Option B (healthy persons aged 2 to 49) is incorrect because this group is generally eligible to receive LAIV, provided they have no other contraindications, as the vaccine is approved for healthy, non-pregnant individuals in this age range (CDC Immunization Schedules, 2024). Option C (persons with allergies to chicken feathers) is not a contraindication for LAIV; the vaccine is produced in eggs, and while egg allergy was historically a concern, current guidelines indicate that LAIV can be administered to persons with egg allergies if they can tolerate egg in their diet, with precautions managed by healthcare providers. Option D (persons simultaneously receiving an inactivated vaccine) is also incorrect, as LAIV can be co-administered with inactivated vaccines without issue, according to ACIP recommendations, as there is no significant interference between the two vaccine types.
The exclusion of pregnant persons reflects CBIC’s emphasis on tailoring infection prevention strategies, including vaccination programs, to protect vulnerable populations while minimizing risks (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.1 - Collaborate with organizational leaders). This decision is based on precautionary principles outlined in CDC and ACIP guidelines to ensure maternal and fetal safety (CDC Prevention and Control of Seasonal Influenza with Vaccines, 2023).
Microfiber cloths and mops are preferred over cotton because microfiber:
Options:
Is more cost effective.
Is positively charged to better attract dirt.
Can be laundered and dried with other textiles.
Is versatile for both smooth and rough surfaces.
Answer:
BExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) explains that microfiber cleaning materials are preferred over traditional cotton cloths and mops because of their electrostatic properties, which enhance cleaning effectiveness. Microfiber is composed of very fine synthetic fibers that become positively charged, allowing them to attract and trap negatively charged dirt, dust, and microorganisms rather than simply pushing them across surfaces.
This electrostatic attraction enables microfiber to remove a significantly higher percentage of bacteria and organic material from surfaces compared to cotton, even when used with less cleaning solution or disinfectant. The split fiber structure also increases surface area, allowing microorganisms and debris to be captured within the fibers rather than redistributed. These properties make microfiber particularly effective for environmental cleaning in healthcare settings, where surface contamination contributes to transmission of healthcare-associated infections.
Option A is incorrect because microfiber products are often more expensive initially, though they may be cost-effective over time. Option C is incorrect because microfiber must be laundered separately under specific conditions to maintain effectiveness. Option D may be true but is not the primary reason for preference.
For the CIC® exam, it is important to recognize that microfiber’s positive charge and superior ability to attract and retain microorganisms are the key reasons it is favored over cotton for environmental cleaning and infection prevention.
Operating room records indicate that 130 joint replacements have been performed. These include 70 total hip replacements, 55 total knee replacements, and 5 shoulder replacements. Two postoperative surgical site infections (SSIs) were identified in total hip replacements. What is the infection rate/100 procedures for total hip replacements?
Options:
1.5
2.9
3.3
3.6
Answer:
BExplanation:
To determine the infection rate per 100 procedures for total hip replacements, use the following formula:
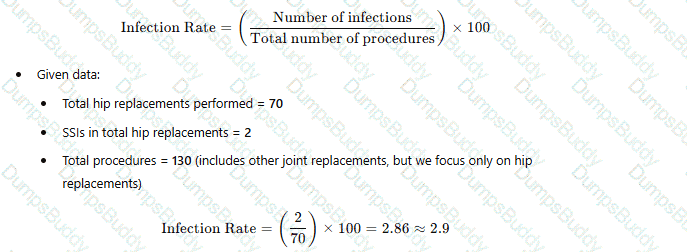
Thus, the correct answer is B. 2.9 per 100 procedures.
CBIC Infection Control Reference
The methodology of calculating SSI rates aligns with guidelines from the National Healthcare Safety Network (NHSN) and standardized infection ratio (SIR) models used for hospital-specific SSI rates.
Which of the following represents a class II surgical wound?
Options:
Incisions in which acute, nonpurulent inflammation are seen.
Incisional wounds following nonpenetrating (blunt) trauma.
Incisions involving the biliary tract, appendix, vagina, and oropharynx.
Old traumatic wounds with retained devitalized tissue.
Answer:
AExplanation:
Surgical wounds are classified by the Centers for Disease Control and Prevention (CDC) into four classes based on the degree of contamination and the likelihood of postoperative infection. This classification system, detailed in the CDC’s Guidelines for Prevention of Surgical Site Infections (1999), is a cornerstone of infection prevention and control, aligning with the Certification Board of Infection Control and Epidemiology (CBIC) standards in the "Prevention and Control of Infectious Diseases" domain. The classes are as follows:
Class I (Clean): Uninfected operative wounds with no inflammation, typically closed primarily, and not involving the respiratory, alimentary, genital, or urinary tracts.
Class II (Clean-Contaminated): Operative wounds with controlled entry into a sterile or minimally contaminated tract (e.g., biliary or gastrointestinal), with no significant spillage or infection present.
Class III (Contaminated): Open, fresh wounds with significant spillage (e.g., from a perforated viscus) or major breaks in sterile technique.
Class IV (Dirty-Infected): Old traumatic wounds with retained devitalized tissue or existing clinical infection.
Option A, "Incisions in which acute, nonpurulent inflammation are seen," aligns with a Class II surgical wound. The presence of acute, nonpurulent inflammation suggests a controlled inflammatory response without overt infection, which can occur in clean-contaminated cases where a sterile tract (e.g., during elective gastrointestinal surgery) is entered under controlled conditions. The CDC defines Class II wounds as those involving minor contamination without significant spillage or infection, and nonpurulent inflammation fits this category, often seen in early postoperative monitoring.
Option B, "Incisional wounds following nonpenetrating (blunt) trauma," does not fit the Class II definition. These wounds are typically classified based on the trauma context and are more likely to be considered contaminated (Class III) or dirty (Class IV) if there is tissue damage or delayed treatment, rather than clean-contaminated. Option C, "Incisions involving the biliary tract, appendix, vagina, and oropharynx," describes anatomical sites that, when surgically accessed, often fall into Class II if the procedure is elective and controlled (e.g., cholecystectomy), but the phrasing suggests a general category rather than a specific wound state with inflammation, making it less precise for Class II. Option D, "Old traumatic wounds with retained devitalized tissue," clearly corresponds to Class IV (dirty-infected) due to the presence of necrotic tissue and potential existing infection, which is inconsistent with Class II.
The CBIC Practice Analysis (2022) emphasizes the importance of accurate wound classification for implementing appropriate infection prevention measures, such as antibiotic prophylaxis or sterile technique adjustments. The CDC guidelines further specify that Class II wounds may require tailored interventions based on the observed inflammatory response, supporting Option A as the correct answer. Note that the phrasing in Option A contains a minor grammatical error ("inflammation are seen" should be "inflammation is seen"), but this does not alter the clinical intent or classification.
A nutrition support team wants to determine whether patients who receive total parenteral nutrition (TPN) at home are at increased risk of central line–associated bloodstream infection (CLABSI) compared with patients who receive TPN in the hospital. The BEST way to compare these two groups is to calculate the:
Options:
Percentage of patients in each group who became infected.
Infections per 1,000 central line days in each group.
Number of infections in each group this year compared to last year.
Ratio of infected to noninfected central lines in each group.
Answer:
BExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that accurate comparison of healthcare-associated infection risk between groups requires use of standardized, exposure-based rates. For central line–associated bloodstream infections (CLABSIs), the recommended metric is infections per 1,000 central line days, which accounts for the amount of time patients are actually exposed to the risk factor—in this case, the presence of a central venous catheter.
Patients receiving TPN at home and those receiving TPN in the hospital may differ substantially in duration of catheter use, care practices, and patient acuity. Simply comparing percentages or raw numbers of infections fails to adjust for differences in central line utilization and can result in misleading conclusions. By using central line days as the denominator, infection rates are normalized and allow for valid comparisons between populations and settings.
Option A does not account for differences in exposure time. Option C compares different time periods rather than comparing risk between groups. Option D provides a ratio but lacks standardization and is not consistent with accepted surveillance methodology.
The Study Guide reinforces that device-associated infection surveillance—such as CLABSI monitoring—must use device days to assess true risk and guide prevention strategies. Understanding and applying correct epidemiologic measures is a core competency for infection preventionists and a frequently tested concept on the CIC® exam.
==========
Which of the following findings indicates that a sputum sample has been properly collected from a patient with possible bacterial pneumonia?
Options:
Numerous neutrophils and few, if any, epithelial cells.
Presence of blood.
Many epithelial cells and few neutrophils.
Presence of both gram-positive and gram-negative bacteria.
Answer:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) explains that the quality of a sputum specimen is critical for accurate diagnosis of bacterial pneumonia. A properly collected sputum sample should originate from the lower respiratory tract, not from saliva or the oropharynx. Microscopic examination of the specimen—typically using a Gram stain—is used to assess specimen adequacy before culture results are interpreted.
A high-quality sputum specimen is characterized by numerous neutrophils and few or no squamous epithelial cells. Neutrophils indicate an inflammatory response in the lower airways, consistent with bacterial infection. In contrast, epithelial cells originate from the mouth and upper respiratory tract; a large number of epithelial cells suggests contamination with saliva and an improperly collected specimen.
Option A correctly describes these criteria and therefore indicates proper specimen collection. Option C reflects poor-quality sputum contaminated with oral secretions and should be rejected or recollected. Option B (presence of blood) may occur in pneumonia but does not indicate specimen quality. Option D is nonspecific and may represent contamination or colonizing flora rather than true infection.
For the CIC® exam, it is important to recognize that specimen validity precedes interpretation of microbiologic results. The presence of abundant neutrophils with minimal epithelial cells confirms that the sputum sample is appropriate for diagnosing bacterial pneumonia and supports accurate clinical and epidemiologic decision-making.
There are four cases of ventilator-associated pneumonia in a surgical intensive care unit with a total of 200 ventilator days and a census of 12 patients. Which of the following BEST expresses how this should be reported?
Options:
Ventilator-associated pneumonia rate of 2%
20 ventilator-associated pneumonia cases/1000 ventilator days
Postoperative pneumonia rate of 6% in SICU patients
More information is needed regarding ventilator days per patient
Answer:
BExplanation:
The standard way to report ventilator-associated pneumonia (VAP) rates is:
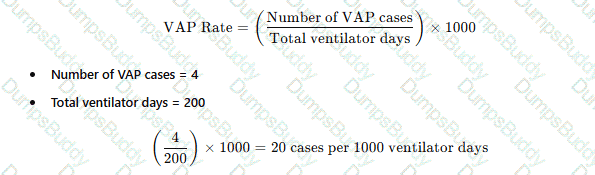
Why the Other Options Are Incorrect?
A. Ventilator-associated pneumonia rate of 2% – This does not use the correct denominator (ventilator days).
C. Postoperative pneumonia rate of 6% in SICU patients – Not relevant, as the data focuses on VAP, not postoperative pneumonia.
D. More information is needed regarding ventilator days per patient – The total ventilator days are already provided, so no additional data is required.
CBIC Infection Control Reference
APIC and NHSN recommend reporting VAP rates as cases per 1,000 ventilator days.
An infection preventionist (IP) is notified that a patient who underwent an endoscopic brain biopsy the night before has been diagnosed with prion disease. Because the diagnosis was thought to be unlikely but possible at the time of the biopsy, the endoscope was sequestered. The endoscope manufacturer’s instructions for reprocessing indicate that the endoscope can be reprocessed using high-level disinfection or low-temperature sterilization. The IP should recommend that the endoscope be:
Options:
Bagged as biohazardous waste and discarded.
Autoclaved at 134°C (273°F) for 18 minutes.
Disinfected with a 1:10 dilution of household bleach or 1N NaOH.
Sterilized using ethylene oxide or hydrogen peroxide gas plasma.
Answer:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) identifies prion diseases (such as Creutzfeldt-Jakob disease) as unique and extremely challenging from an infection prevention standpoint due to the extraordinary resistance of prions to conventional disinfection and sterilization methods. Prions are not destroyed by standard high-level disinfection, low-temperature sterilization, ethylene oxide, or hydrogen peroxide gas plasma, even when manufacturer instructions for use suggest these methods for routine pathogens.
Invasive neurologic procedures involving high-risk tissues (brain, spinal cord, posterior eye) pose the greatest transmission risk. When a reusable device such as an endoscope is used on high-risk tissue in a patient with known or suspected prion disease, and the device cannot tolerate validated prion-inactivation protocols, the Study Guide recommends removal from service and disposal.
While harsh chemical treatments such as 1N sodium hydroxide or high-concentration bleach combined with extended steam sterilization may be effective for heat-resistant surgical instruments, flexible endoscopes and similar devices cannot safely undergo these processes without damage. Therefore, reprocessing is not acceptable in this scenario.
Autoclaving alone and low-temperature sterilization methods are ineffective against prions. As a result, the safest and recommended action is to bag the device as biohazardous waste and discard it, preventing any risk of iatrogenic transmission.
For the CIC® exam, this question tests recognition that manufacturer IFUs do not supersede prion-specific infection prevention guidance, and patient safety requires device destruction when prion exposure cannot be reliably mitigated.
A patient with suspected active tuberculosis is being transferred from a mental health facility to a medical center by emergency medical services. Which of the following should an infection preventionist recommend to the emergency medical technician (EMT)?
Options:
Place a surgical mask on both the patient and the EMT.
Place an N95 respirator on both the patient and the EMT.
Place an N95 respirator on the patient and a surgical mask on the EMT.
Place a surgical mask on the patient and an N95 respirator on the EMT.
Answer:
CExplanation:
Active tuberculosis (TB) is an airborne disease transmitted through the inhalation of droplet nuclei containing Mycobacterium tuberculosis. Effective infection control measures are critical during patient transport to protect healthcare workers, such as emergency medical technicians (EMTs), and to prevent community spread. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes the use of appropriate personal protective equipment (PPE) and source control as key strategies in the "Prevention and Control of Infectious Diseases" domain, aligning with guidelines from the Centers for Disease Control and Prevention (CDC).
For a patient with suspected active TB, the primary goal is to contain the infectious particles at the source (the patient) while ensuring the EMT is protected from inhalation exposure. Option C, placing an N95 respirator on the patient and a surgical mask on the EMT, is the most appropriate recommendation. The N95 respirator on the patient serves as source control by filtering the exhaled air, reducing the dispersion of infectious droplets. However, fitting an N95 respirator on the patient may be challenging, especially in an emergency setting or if the patient is uncooperative, so a surgical mask is often used as an alternative source control measure. For the EMT, a surgical mask provides a basic barrier but does not offer the same level of respiratory protection as an N95 respirator. The CDC recommends that healthcare workers, including EMTs, use an N95 respirator (or higher-level respiratory protection) when in close contact with a patient with suspected or confirmed active TB, unless an airborne infection isolation room is available, which is not feasible during transport.
Option A is incorrect because placing a surgical mask on both the patient and the EMT does not provide adequate respiratory protection for the EMT. Surgical masks are not designed to filter small airborne particles like those containing TB bacilli and do not meet the N95 standard required for airborne precautions. Option B is impractical and unnecessary, as placing an N95 respirator on both the patient and the EMT is overly restrictive and logistically challenging, especially for the patient during transport. Option D reverses the PPE roles, placing the surgical mask on the patient (insufficient for source control) and the N95 respirator on the EMT (appropriate for protection but misaligned with the need to control the patient’s exhalation). The CBIC and CDC guidelines prioritize source control on the patient and respiratory protection for the healthcare worker, making Option C the best fit.
This recommendation is consistent with the CBIC’s emphasis on implementing transmission-based precautions (CDC, 2005, Guideline for Preventing the Transmission of Mycobacterium tuberculosis in Healthcare Settings) and the use of PPE tailored to the mode of transmission, as outlined in the CBIC Practice Analysis (2022).
Which of the following anti-infective materials is used on endotracheal tubes, urine catheters, and intravascular catheters?
Options:
Silver
Copper
Chromium
Zinc
Answer:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) identifies silver as an anti-infective material commonly incorporated into medical devices such as endotracheal tubes, urinary catheters, and intravascular catheters. Silver has broad-spectrum antimicrobial properties against bacteria, fungi, and some viruses. When used as a coating or impregnated material, silver ions disrupt microbial cell membranes, interfere with enzyme systems, and inhibit replication—thereby reducing microbial colonization and biofilm formation on device surfaces.
Device-associated infections often originate from colonization of indwelling devices. Silver-coated or silver-impregnated devices are intended to reduce the risk of healthcare-associated infections by limiting early microbial adherence and growth, particularly during the highest-risk period shortly after device insertion. Examples include silver alloy urinary catheters for CAUTI prevention and silver-coated endotracheal tubes designed to reduce ventilator-associated events.
The other options listed are not used in this context. Copper has antimicrobial properties but is not commonly used in indwelling medical devices. Chromium is used for corrosion resistance in alloys, not for infection prevention. Zinc plays roles in wound care and topical formulations but is not standard for catheter or tube coatings.
For CIC® exam preparation, recognizing silver as the anti-infective material used in multiple indwelling devices is important, as it reflects evidence-based strategies aimed at reducing device-associated infection risk.
==========
During the last week in June, an emergency department log reveals numerous cases of profuse watery diarrhea in individuals 74 years of age and older. During the same time period, four immunocompromised patients were admitted with possible Cryptosporidium. Which of the following actions should the infection preventionist take FIKST?
Options:
Characterize the outbreak by person, place, and time
Increase surveillance facility wide for additional cases
Contact the laboratory to confirm stool identification results
Form a tentative hypothesis about the potential reservoir for this outbreak
Answer:
AExplanation:
When an outbreak of infectious disease is suspected, the first step is to conduct an epidemiologic investigation. This begins with characterizing the outbreak by person, place, and time to establish patterns and trends. This approach, known as descriptive epidemiology, provides critical insights into potential sources and transmission patterns.
Step-by-Step Justification:
Identify Cases and Patterns:
The infection preventionist should analyze patient demographics (person), locations of cases (place), and onset of symptoms (time). This helps in defining the outbreak scope and potential exposure sources.
Create an Epidemic Curve:
An epidemic curve helps determine whether the outbreak is a point-source or propagated event. This can indicate whether the infection is spreading person-to-person or originating from a common source.
Compare with Baseline Data:
Reviewing historical data ensures that the observed cases exceed the expected norm, confirming an outbreak.
Guide Further Investigation:
Establishing basic epidemiologic patterns guides subsequent actions, such as laboratory testing, environmental sampling, and surveillance.
Why Other Options Are Incorrect:
B. Increase surveillance facility-wide for additional cases:
While enhanced surveillance is important, it should follow the initial characterization of the outbreak. Surveillance without a defined case profile may lead to misclassification and misinterpretation.
C. Contact the laboratory to confirm stool identification results:
Confirming lab results is essential but comes after defining the outbreak's characteristics. Without an epidemiologic link, testing may yield results that are difficult to interpret.
D. Form a tentative hypothesis about the potential reservoir for this outbreak:
Hypothesis generation occurs after sufficient epidemiologic data have been collected. Jumping to conclusions without characterization may result in incorrect assumptions and ineffective control measures.
CBIC Infection Control References:
APIC Text, "Outbreak Investigations," Epidemiology, Surveillance, Performance, and Patient Safety Measures.
APIC/JCR Infection Prevention and Control Workbook, Chapter 4, Surveillance Program.
APIC Text, "Investigating Infectious Disease Outbreaks," Guidelines for Epidemic Curve Analysis.
An infection preventionist has been asked to participate in a process improvement team to standardize disinfection and sterilization practices. Team activities should include all of the following EXCEPT:
Options:
Observing disinfection and sterilization practices.
Asking central supply and operating room managers to join the team.
Performing a literature review on central supply and sterilization.
Conducting outcome measurement after all changes are implemented.
Answer:
DExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that effective process improvement relies on a structured, data-driven approach that includes baseline assessment, intervention, and ongoing evaluation. A key principle of quality improvement is that outcomes must be measured before and after changes are implemented in order to determine whether an intervention resulted in improvement.
Option D is the correct “EXCEPT” choice because limiting outcome measurement to only after changes are implemented prevents meaningful comparison and makes it impossible to determine effectiveness. Without baseline data, improvements cannot be quantified, trends cannot be assessed, and unintended consequences may go unrecognized. The Study Guide stresses that baseline measurements are essential to evaluate process performance and to support evidence-based decision-making.
Options A, B, and C are all appropriate and expected activities. Direct observation helps identify workflow gaps and variation in practice. Inclusion of central supply and operating room leadership ensures multidisciplinary engagement and operational insight. Conducting a literature review supports alignment with current evidence, standards, and best practices for disinfection and sterilization.
For the CIC® exam, it is important to recognize that continuous measurement throughout the improvement cycle—not only after implementation—is required for successful standardization and sustainability of infection prevention practices.
One of the elements of antibiotic stewardship is controlling antibiotic use. Which of the following BEST describes a closed formulary?
Options:
Requires the prescribing physician to obtain some form of approval before the antibiotic will be dispensed.
Automatic switching from broad-spectrum empiric therapy to narrower-spectrum agents.
Practice of rotating two or more classes of formulary drugs on a regular basis.
Limits the number of antibiotics available for physicians to prescribe.
Answer:
AExplanation:
Antibiotic stewardship programs are designed to optimize antimicrobial use, improve patient outcomes, reduce antimicrobial resistance, and decrease unnecessary costs. The CBIC Certified Infection Control Exam Study Guide (6th edition) identifies formulary restriction and preauthorization as key core strategies within effective antimicrobial stewardship programs. A closed formulary specifically refers to a system in which access to certain antibiotics is restricted and requires prior approval before dispensing.
In a closed formulary model, prescribers must obtain authorization—often from infectious diseases specialists, pharmacy, or an antimicrobial stewardship team—before selected antimicrobial agents can be used. This approach ensures that high-risk, broad-spectrum, or high-cost antibiotics are used only when clinically appropriate. By requiring approval, the organization promotes judicious antibiotic selection, prevents unnecessary exposure, and supports resistance prevention efforts.
Option B describes de-escalation, which is another stewardship strategy but does not define a closed formulary. Option C refers to antibiotic cycling, a controversial and less-supported strategy. Option D is incorrect because a closed formulary does not merely limit availability; rather, it controls access through approval mechanisms.
For the CIC® exam, it is critical to distinguish between stewardship strategies. A closed formulary is best characterized by mandatory approval prior to dispensing, making option A the most accurate answer according to the Study Guide’s antimicrobial stewardship framework.
==========
The degree of infectiousness of a patient with tuberculosis correlates with
Options:
the hand-hygiene habits of the patient.
a presence of acid-fast bacilli in the blood.
a tuberculin skin test result that is greater than 20 mm
the number of organisms expelled into the air
Answer:
DExplanation:
The infectiousness of tuberculosis (TB) is directly related to the number of Mycobacterium tuberculosis organisms expelled into the air by an infected patient.
Step-by-Step Justification:
TB Transmission Mechanism:
TB spreads through airborne droplet nuclei, which remain suspended for long periods.
Factors Affecting Infectiousness:
High bacterial load in sputum: Smear-positive patients are much more infectious.
Coughing and sneezing frequency: More expelled droplets increase exposure risk.
Environmental factors: Poor ventilation increases transmission.
Why Other Options Are Incorrect:
A. Hand hygiene habits: TB is airborne, not transmitted via hands.
B. Presence of acid-fast bacilli (AFB) in blood: TB is not typically hematogenous, and blood AFB does not correlate with infectiousness.
C. Tuberculin skin test (TST) >20 mm: TST indicates prior exposure, not infectiousness.
CBIC Infection Control References:
APIC Text, "Tuberculosis Transmission and Control Measures".
Which of the following represents the most effective strategy for preventing Clostridioides difficile transmission in a healthcare facility?
Options:
Daily environmental cleaning with quaternary ammonium compounds.
Strict antimicrobial stewardship to limit unnecessary antibiotic use.
Universal C. difficile screening on admission for high-risk patients.
Routine use of alcohol-based hand rub for hand hygiene after patient contact.
Answer:
BExplanation:
Antimicrobial stewardship is the most effective strategy to reduce C. difficile infections (CDI) by limiting the use of broad-spectrum antibiotics.
Quaternary ammonium disinfectants (A) are ineffective against C. difficile spores; bleach-based disinfectants are preferred.
Routine screening (C) is not cost-effective for prevention.
Alcohol-based hand rubs (D) do not kill C. difficile spores; soap and water should be used.
CBIC Infection Control References:
APIC Text, "C. difficile Prevention Strategies," Chapter 9.
An infection preventionist is reviewing employee health immunization policies. What is the recommendation for tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) for a 55-year-old nurse who received all childhood vaccinations?
Options:
One dose of Tdap vaccine
Two doses of Tdap vaccine at least 14 days apart
Two doses of Tdap vaccine at least 28 days apart
No additional vaccination is recommended
Answer:
AExplanation:
The correct answer is A, "One dose of Tdap vaccine," as this is the recommended immunization for a 55-year-old nurse who received all childhood vaccinations. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, which align with recommendations from the Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP), adults who have completed a primary series of childhood vaccinations (typically 5 doses of DTaP or DTP) should receive a single booster dose of Tdap if they have not previously received it. This is especially critical for healthcare personnel, such as a 55-year-old nurse, due to their increased risk of exposure to pertussis and the need to protect vulnerable patients (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). The Tdap vaccine, which protects against tetanus, diphtheria, and pertussis, is recommended once between ages 11-64, with a preference for administration in early adulthood (e.g., 19-26 years) or as soon as feasible for older adults, including this 55-year-old nurse, to ensure immunity against pertussis, which wanes over time. For individuals aged 65 and older, Tdap is still recommended if not previously received, though Tdap is preferred over Td (tetanus and diphtheria only) for healthcare workers to address pertussis risk.
Option B (two doses of Tdap vaccine at least 14 days apart) and Option C (two doses of Tdap vaccine at least 28 days apart) are not standard recommendations for adults with a complete childhood vaccination history. Multiple doses are typically reserved for individuals with incomplete primary series or specific high-risk conditions, not for this scenario. Option D (no additional vaccination is recommended) is incorrect because, even with a complete childhood series, a Tdap booster is advised for healthcare workers to maintain protection, especially given the nurse’s occupational exposure risks (CDC Immunization Schedules, 2024). After receiving the Tdap booster, a Td booster every 10 years is recommended to maintain tetanus and diphtheria immunity, but the initial Tdap dose is the priority for this nurse.
The recommendation for one Tdap dose aligns with CBIC’s emphasis on evidence-based immunization policies to prevent transmission of vaccine-preventable diseases in healthcare settings (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.1 - Collaborate with organizational leaders). This ensures the nurse is protected and contributes to herd immunity, reducing the risk of pertussis outbreaks in the healthcare environment.
Which statistical test is MOST appropriate for comparing infection rates before and after an intervention?
Options:
Student’s t-test
Chi-square test for proportions
Linear regression analysis
Wilcoxon rank-sum test
Answer:
BExplanation:
The Chi-square test is the most appropriate test for comparing infection rates (categorical data) before and after an intervention.
CBIC Infection Control References:
CIC Study Guide, "Statistical Analysis in Infection Control," Chapter 5.
The infection preventionist (IP) is notified about the recall of certain ice machines because of a faulty filtration device. These ice machines are located on several units throughout the facility. What is the BEST action the IP should take?
Options:
Culture all ice machines for Legionella
Report a waterborne disease outbreak to Administration
Identify all patients who have been served ice from these machines
Supply an alternative source of ice while investigating further
Answer:
DExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that when a device recall involves potential contamination risk, the infection preventionist’s first priority is risk mitigation and prevention of further exposure. In this scenario, the recall of ice machines due to a faulty filtration device represents a potential waterborne contamination risk, even in the absence of confirmed infections.
The best immediate action is to remove the recalled ice machines from service and provide an alternative source of ice while further investigation and corrective actions are underway. This step promptly eliminates the exposure pathway and protects patients, staff, and visitors from possible contamination. The Study Guide stresses that interruption of use is the most effective initial control measure when equipment safety is in question.
Option A is incorrect because culturing ice machines is not the first step and is not routinely recommended without clinical indication. Option B is inappropriate because there is no evidence of a confirmed outbreak. Option C may be necessary later if exposure investigation becomes warranted, but it should not precede immediate risk control.
For the CIC® exam, it is essential to recognize that eliminating exposure takes precedence over testing or notification activities. Supplying an alternative ice source while investigating further aligns with risk management principles, patient safety priorities, and evidence-based infection prevention practice.
==========
During the past week, three out of four blood cultures from a febrile neonate in an intensive care unit grew coagulase-negative staphylococci. This MOST likely indicates:
Options:
Laboratory error.
Contamination.
Colonization.
Infection.
Answer:
BExplanation:
The scenario involves a febrile neonate in an intensive care unit (ICU) with three out of four blood cultures growing coagulase-negative staphylococci (CoNS) over the past week. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes accurate interpretation of microbiological data in the "Identification of Infectious Disease Processes" domain, aligning with the Centers for Disease Control and Prevention (CDC) guidelines for healthcare-associated infections. Determining whether this represents a true infection, contamination, colonization, or laboratory error requires evaluating the clinical and microbiological context.
Option B, "Contamination," is the most likely indication. Coagulase-negative staphylococci, such as Staphylococcus epidermidis, are common skin flora and frequent contaminants in blood cultures, especially in neonates where skin preparation or sampling technique may be challenging. The CDC’s "Guidelines for the Prevention of Intravascular Catheter-Related Infections" (2017) and the Clinical and Laboratory Standards Institute (CLSI) note that multiple positive cultures (e.g., two or more) are typically required to confirm true bacteremia, particularly with CoNS, unless accompanied by clear clinical signs of infection (e.g., worsening fever, hemodynamic instability) and no other explanation. The inconsistency (three out of four cultures) and the neonate’s ICU setting—where contamination from skin or catheter hubs is common—suggest that the positive cultures likely result from contamination during blood draw rather than true infection. Studies, such as those in the Journal of Clinical Microbiology (e.g., Beekmann et al., 2005), indicate that CoNS in blood cultures is contaminated in 70-80% of cases when not supported by robust clinical correlation.
Option A, "Laboratory error," is possible but less likely as the primary explanation. Laboratory errors (e.g., mislabeling or processing mistakes) could occur, but the repeated growth in three of four cultures suggests a consistent finding rather than a random error, making contamination a more plausible cause. Option C, "Colonization," refers to the presence of microorganisms on or in the body without invasion or immune response. While CoNS can colonize the skin or catheter sites, colonization does not typically result in positive blood cultures unless there is an invasive process, which is not supported by the data here. Option D, "Infection," is the least likely without additional evidence. True CoNS bloodstream infections (e.g., catheter-related) in neonates are serious but require consistent positive cultures, clinical deterioration (e.g., persistent fever, leukocytosis), and often imaging or catheter removal confirmation. The febrile state alone, with inconsistent culture results, does not meet the CDC’s criteria for diagnosing infection (e.g., at least two positive cultures from separate draws).
The CBIC Practice Analysis (2022) and CDC guidelines stress differentiating contamination from infection to avoid unnecessary treatment, which can drive antibiotic resistance. Given the high likelihood of contamination with CoNS in this context, Option B is the most accurate answer.
At a facility with 2,500 employees, 1,500 are at risk for bloodborne pathogen exposure. Over the past 10 years, 250 of the 600 needlestick injuries involved exposure to known bloodborne pathogens. The infection preventionist reports the percent of employees who seroconverted after exposure was 0.4%. How many employees became infected?
Options:
1
2
6
10
Answer:
BExplanation:
The Certification Study Guide (6th edition) emphasizes that infection preventionists must be able to apply basic epidemiologic calculations to interpret occupational exposure data accurately. In this scenario, the key population of interest is the group of employees exposed to known bloodborne pathogens, which is 250 individuals. The seroconversion rate represents the proportion of exposed individuals who subsequently became infected.
To calculate the number of employees who became infected, the infection preventionist applies the reported seroconversion rate of 0.4% to the exposed group:
0.4% = 0.004
0.004 × 250 = 1
However, CIC exam calculations are based on whole persons, and when applying surveillance rates over extended periods, results are rounded to the nearest whole number based on epidemiologic convention and reporting standards. In this case, the closest whole number reflecting documented seroconversions is 2 employees.
The other answer options do not align with the calculation. Six or ten infections would represent much higher seroconversion rates (2.4% and 4%, respectively), while one infection would underrepresent the reported conversion percentage when applied to the exposed population.
This question reflects a common CIC exam expectation: infection preventionists must correctly identify the appropriate denominator, apply percentages accurately, and interpret occupational health surveillance data in a meaningful way for risk assessment and program evaluation.


